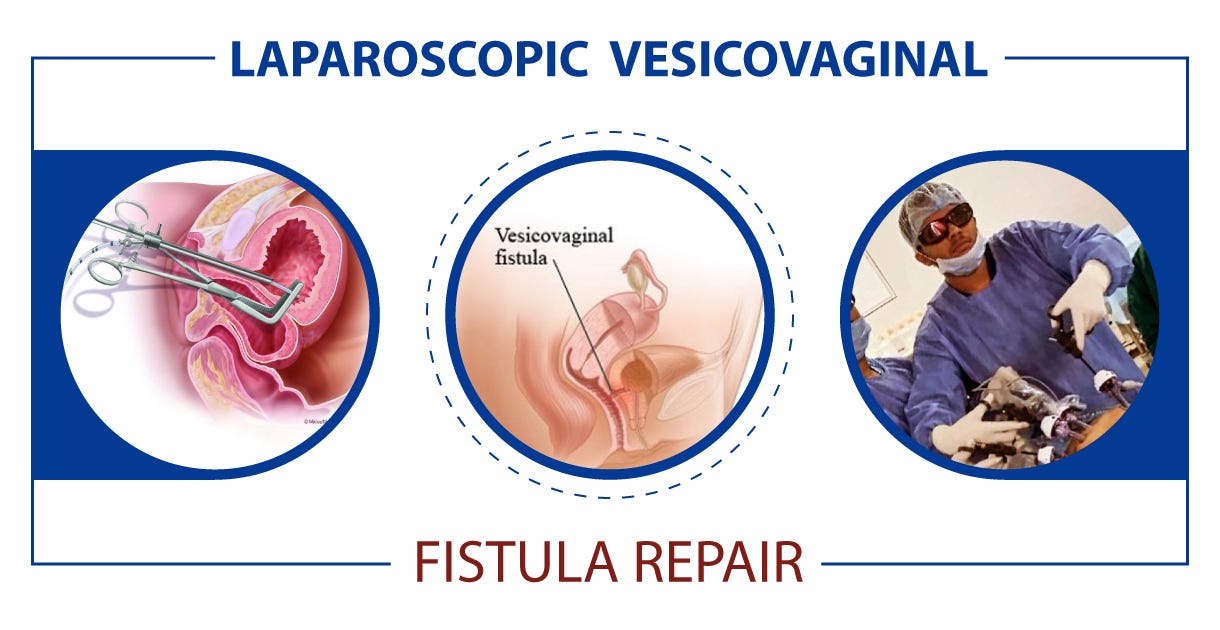
Imagine living with the constant discomfort of a vesicovaginal fistula, an abnormal connection between the bladder and vagina.
The physical and emotional struggle is overwhelming.
But fear not, because there is hope.
In this article, we will explore the fascinating world of vesicovaginal fistula repair, uncovering the intricate surgical procedures and innovative techniques that can restore your quality of life.
So grab a comfortable seat and get ready to be amazed by the incredible resilience of the human body and modern medical advancements.
repair of vesicovaginal fistula
The repair of a vesicovaginal fistula is a surgical procedure that aims to close or remove a fistula, which is an abnormal opening, between the bladder and vagina.
This procedure is performed under general anesthesia, and various techniques may be used, including excising or closing the fistula with stitches.
To prevent infection, patients may be instructed to fast and use a specific soap before surgery, and antibiotic-soaked bandages may be placed in the vagina afterwards.
Risks of the surgery include bleeding, infection, damage to the ureters, and the possibility of a new fistula forming.
Success in the repair is achieved by following certain surgical principles, and in some cases, additional techniques may be required for radiation patients.
Different incisions and approaches may be used depending on the specific case, and vascularized flaps or grafts may be utilized for larger or radiotherapy-related fistulas.
Overall, with proper surgical technique, the success rates for vesicovaginal fistula repair are high.
Key Points:
- Repair of vesicovaginal fistula aims to close or remove an abnormal opening between the bladder and vagina.
- The procedure is performed under general anesthesia and can involve excising or closing the fistula with stitches.
- Patients may be instructed to fast and use a specific soap before surgery to prevent infection.
- Risks of the surgery include bleeding, infection, damage to the ureters, and the formation of a new fistula.
- Success in the repair relies on following surgical principles and additional techniques may be needed for radiation patients.
- Different incisions and approaches may be used, and vascularized flaps or grafts may be utilized for larger or radiotherapy-related fistulas.
repair of vesicovaginal fistula – Watch Video
💡
Pro Tips:
1. The earliest known successful repair of a vesicovaginal fistula was performed in ancient Egypt around 1500 BCE by an Egyptian surgeon named Imhotep.
2. Famed American gynecologist Dr. J. Marion Sims is often credited with pioneering the modern surgical techniques for repairing vesicovaginal fistulas. However, the controversial aspect of his work was that he performed these procedures on enslaved African American women without their consent and without using anesthesia.
3. In the early 20th century, many women affected by vesicovaginal fistula sought treatment from traditional healers rather than modern medicine. This was due to a combination of social stigma, lack of awareness about effective surgical treatments, and belief in traditional remedies.
4. Vesicovaginal fistulas can be caused by a variety of factors, including childbirth complications, pelvic surgery, radiation therapy, or injury to the pelvic area.
5. The World Health Organization estimates that around 2 million women in developing countries suffer from obstetric fistulas, including vesicovaginal fistulas. These fistulas often occur as a result of prolonged and obstructed labor without access to timely emergency obstetric care. Efforts are ongoing to increase awareness, accessibility to treatment, and to eradicate this preventable condition.
Pre-Surgery Instructions And Precautions
Before undergoing repair of vesicovaginal fistula surgery, patients are typically provided with pre-surgery instructions and precautions to ensure the procedure is successful and to minimize the risk of complications.
One common instruction is for patients to fast for a certain period of time before the surgery, typically starting at midnight the night before the procedure. This fasting is necessary to prevent any food or drink from interfering with the anesthesia or the surgical process.
In addition to fasting, patients may also be advised to shower with a specific antibacterial soap in the days leading up to the surgery. This is done to reduce the risk of infection at the surgical site. By using an antibacterial soap, patients can help eliminate any potential bacteria on their skin that could potentially enter the surgical incision during the procedure.
Following these pre-surgery instructions is crucial as it helps create a clean and sterile environment for the surgery, reducing the risk of infection and ensuring the best possible outcome for the repair of vesicovaginal fistula.
- Fast starting at midnight the night before the procedure
- Shower with specific antibacterial soap to reduce the risk of infection
Administration Of General Anesthesia
Repair of vesicovaginal fistula is typically performed under general anesthesia. General anesthesia is a type of anesthesia that renders the patient unconscious and immobile during the surgery. This ensures that the patient does not experience any pain or discomfort during the procedure.
The administration of general anesthesia is a critical step in the surgical process as it allows the surgeon to perform the necessary repairs without any interference from the patient. It also ensures that the patient remains completely still, reducing the risk of complications during the surgery.
An anesthesiologist is responsible for administering and monitoring the anesthesia throughout the procedure. They carefully monitor the patient’s vitals, including heart rate, blood pressure, and oxygen levels, to ensure the patient remains stable and safe throughout the operation.
Ureteral Stents For Protection
During the repair of vesicovaginal fistula surgery, surgeons commonly insert ureteral stents. Ureteral stents are small hollow tubes that are placed into the ureters, the tubes connecting the kidneys to the bladder. These stents serve two primary purposes during the surgery:
- Protection: Ureteral stents help protect the ureters from any potential damage during the repair procedure. By placing the stents, the surgeon can ensure that the ureters are not accidentally injured or obstructed during the surgical process.
- Maintaining Urine Flow: Ureteral stents help maintain the normal flow of urine from the kidneys to the bladder. By keeping the ureters open and free from any obstruction, the stents ensure that urine can be properly drained from the kidneys and disposed of through the bladder.
The use of ureteral stents is a common precautionary measure that can help prevent complications during and after the repair of vesicovaginal fistula surgery.
- Blockquote:
“The use of ureteral stents is a common precautionary measure that can help prevent complications during and after the repair of vesicovaginal fistula surgery.”
💡
You may need to know these questions about repair of vesicovaginal fistula
What is the name of the surgery for VVF repair?
The surgical procedure for repairing vesicovaginal fistulae is often referred to as VVF repair surgery. This procedure can be performed through different approaches, including transvaginal or laparoscopic methods. In certain cases, patients who have undergone multiple transvaginal procedures may consider a final repair through a large abdominal incision, known as laparotomy.
How is VVF surgery done?
Vesicovaginal fistula (VVF) surgery is typically performed using laparoscopic techniques, known as keyhole surgery. The procedure involves removing the damaged tissue and closing the fistula with stitches. In some cases, when the surgery is conducted through the vagina, fat from the labia can be utilized to provide additional support to the repair. This technique, called a Martius Flap, enhances the success of the surgery and aids in the healing process.
What is the success rate of VVF repair?
The success rate of repairing nonradiated vesicovaginal fistulas (VVF) ranges from 70% to 100%, with an average success rate of 92%. However, it is important to note that fistulas caused by radiation pose a greater challenge for repair and should not be compared to nonradiated cases. Therefore, the success rates for repairing radiation-induced VVF may differ significantly from the mentioned range for nonradiated cases.
What is the recovery time for VVF surgery?
The recovery time for VVF surgery is relatively short. While patients have a catheter for two to three weeks to facilitate bladder healing, the vaginal incision does not usually result in significant discomfort. Furthermore, patients typically spend only one night in the hospital, indicating a swift recovery process.
Reference source
https://my.clevelandclinic.org/health/diseases/16442-vesicovaginal-fistula
https://en.wikipedia.org/wiki/Vesicovaginal_fistula
https://mft.nhs.uk/app/uploads/sites/4/2018/04/Vesico-Vaginal-Fistula-January-2018.pdf
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4039689/