Infantile Uterus: Understanding the Causes, Symptoms, and Treatments
– Uterine hypoplasia is a condition that affects women’s reproductive health, where the uterus is abnormally small or underdeveloped.
– This condition can cause fertility issues, menstrual irregularities, and difficulties during pregnancy.
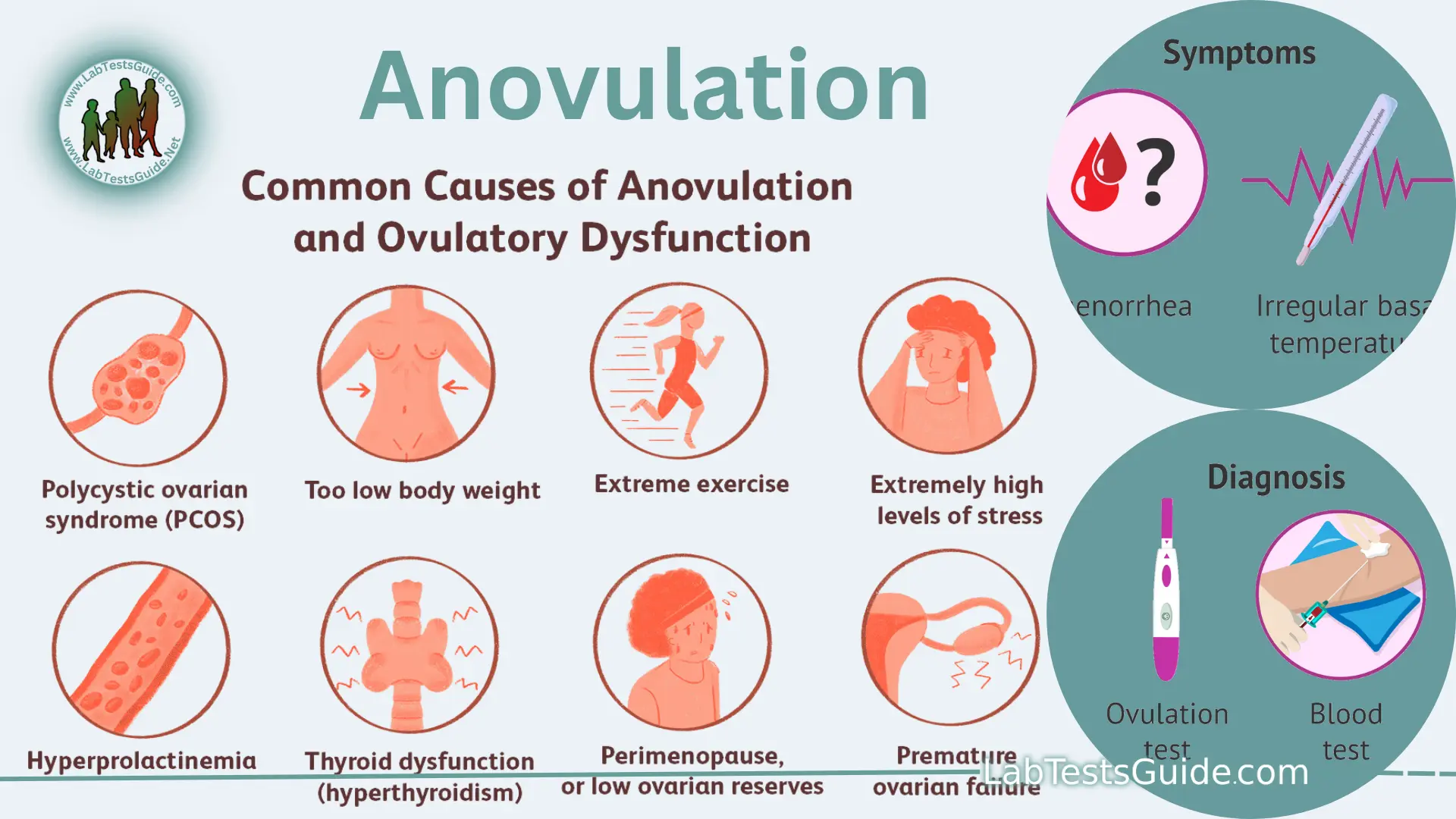
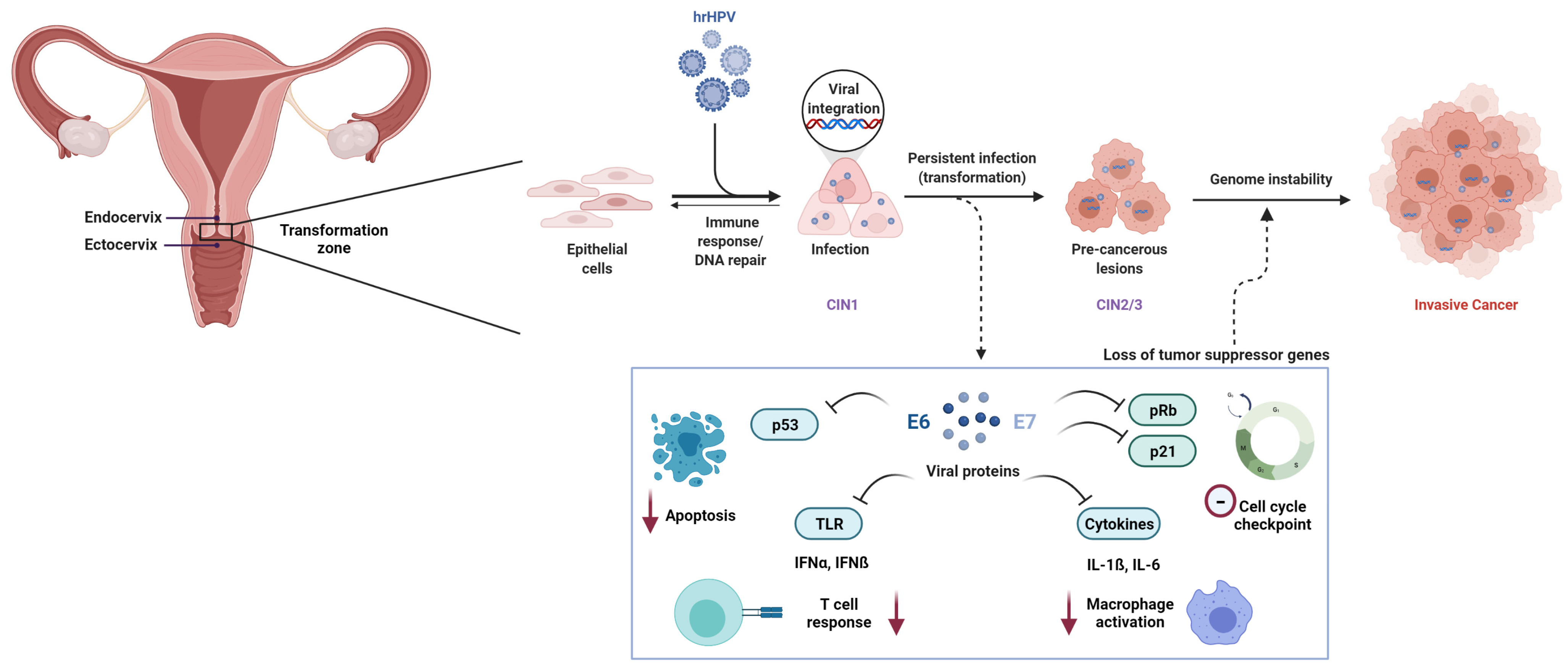
– Causes of uterine hypoplasia can include genetic abnormalities, exposure to toxins, hormonal imbalances, infections or inflammations of the uterus, and past surgeries or other conditions.
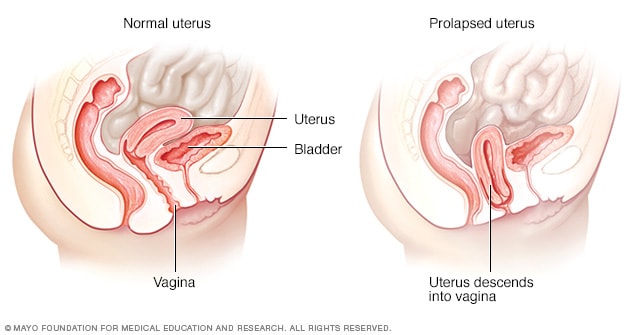
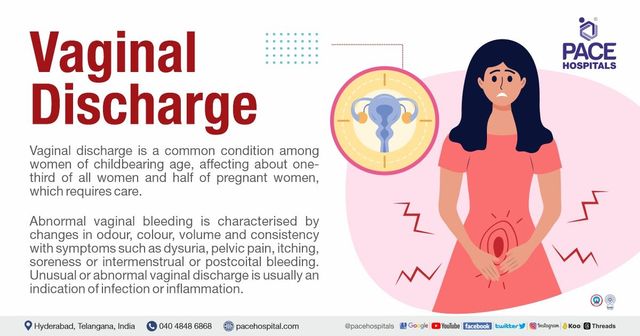
– Symptoms of uterine hypoplasia may include abnormal menstrual cycles, infertility, pelvic pain, and abnormalities detected through imaging tests.
– The severity of symptoms can vary depending on the degree of uterine hypoplasia.
– There are three degrees of uterine hypoplasia: first degree, second degree, and third degree.
– Treatment options for hypoplastic uterus include hormonal medications, intrauterine insemination, in vitro fertilization, surrogacy, uterine reconstruction surgery, and psychological counseling.
– Diagnostic tests that may be performed include ultrasound imaging, hysterosalpingography, and magnetic resonance imaging.
– It is important to consult with a healthcare provider for personalized recommendations based on individual needs and medical history.
– A small uterus refers to a uterus that is smaller than the average size.
– The causes of a small uterus can include genetic factors, congenital disorders, exposure to certain chemicals or radiation, and health issues such as Asherman’s Syndrome or Turner Syndrome.
– Treatment options for a small uterus can vary and commonly involve hormone therapy.
– Women with a small uterus who experience amenorrhea may receive hormonal therapy and further investigation into underlying conditions.
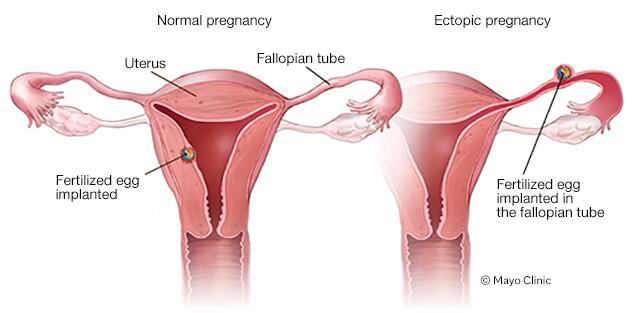
– Pregnancy without a uterus is possible through gestational surrogacy.
– A small uterus can present challenges during pregnancy, but with regular prenatal care and personalized care plans, successful pregnancies can still occur.
– With the right care and fertility treatments, dreams of parenthood can be realized.