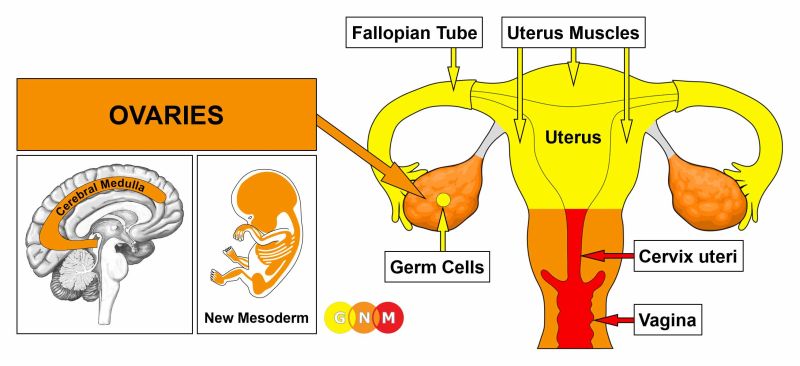
– Endometrioid cancer is the most common type of cancer in the uterus and starts in the inner lining of the uterus (endometrium).
– There are different types of endometrial cancers, including adenocarcinoma (most common), uterine carcinosarcoma, squamous cell carcinoma, small cell carcinoma, transitional carcinoma, serous carcinoma, clear-cell carcinoma, mucinous adenocarcinoma, undifferentiated carcinoma, dedifferentiated carcinoma, and serous adenocarcinoma.
– Endometrioid cancer starts in gland cells and resembles the normal uterine lining.
– Some endometrioid cancers have squamous cells in addition to glandular cells.
– There are several sub-types of endometrioid cancers, including adenocarcinoma (with squamous differentiation), adenoacanthoma, adenosquamous (or mixed cell), secretory carcinoma, ciliated carcinoma, and villoglandular adenocarcinoma.
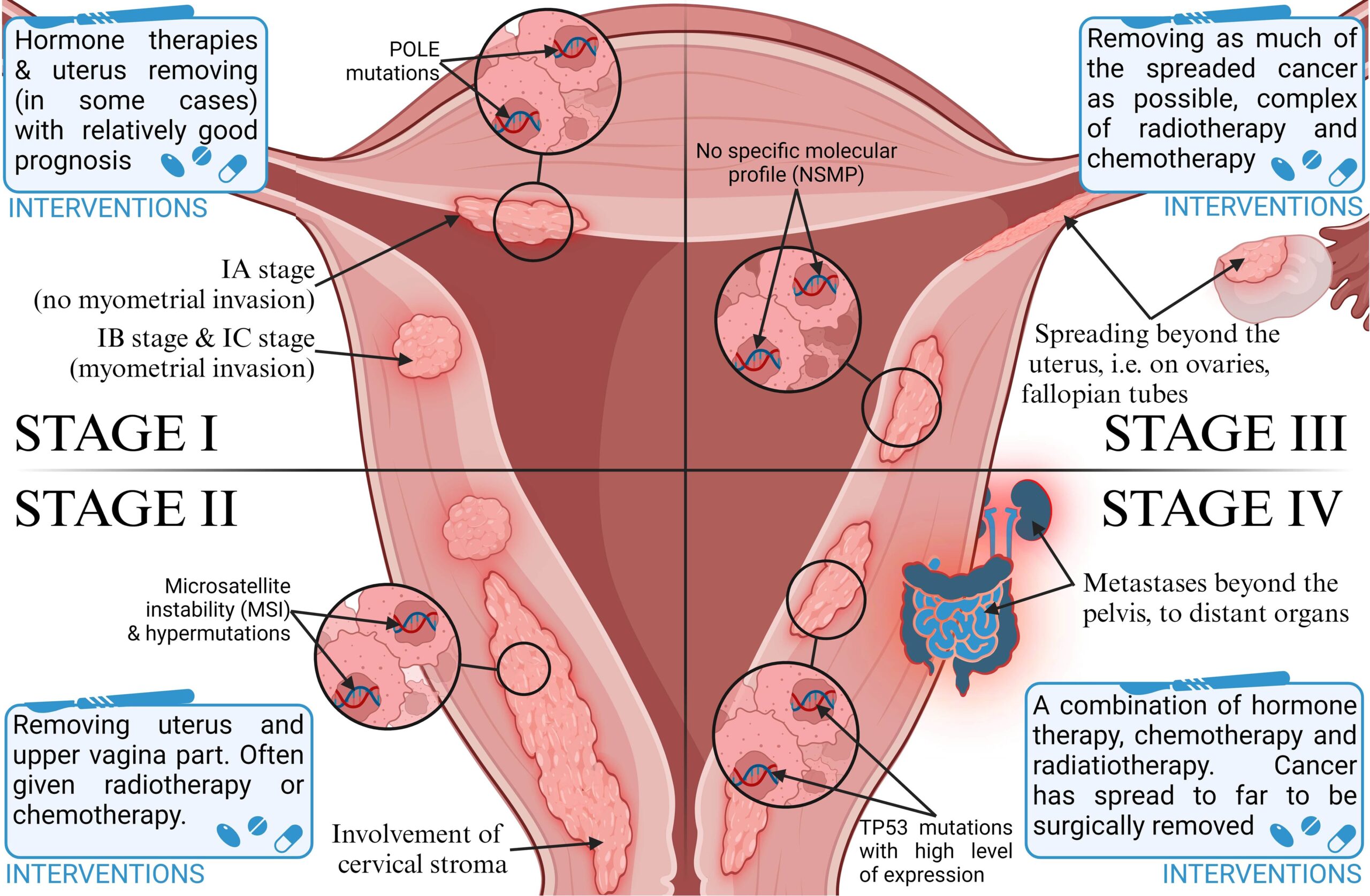
– The grade of an endometrial cancer is determined by the organization of the cancer cells into gland-like structures.
– Grade 1 tumors of endometrioid cancer have 95% or more of the cancer tissue forming glands.
– Grade 2 tumors have between 50% and 94% of the cancer tissue forming glands.
– Grade 3 tumors have less than half of the cancer tissue forming glands and tend to be aggressive with a worse outlook.
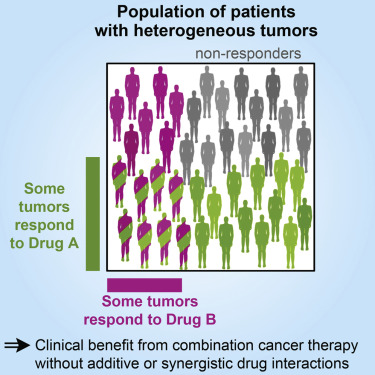
– Type 1 endometrial cancers are usually not aggressive and are caused by too much estrogen. They may develop from atypical hyperplasia.
– Type 2 endometrial cancers are more likely to grow and spread outside the uterus and have a poorer outlook. They are not caused by too much estrogen and include papillary serous carcinoma, clear-cell carcinoma, undifferentiated carcinoma, and grade 3 endometrioid carcinoma.
– Uterine carcinosarcoma (CS) starts in the endometrium and has features of both endometrial carcinoma and sarcoma. It is a type 2 endometrial carcinoma.
– Uterine sarcomas start in the muscle layer or supporting connective tissue of the uterus.
– Cancers that start in the cervix and spread to the uterus are different from cancers that start in the body of the uterus.
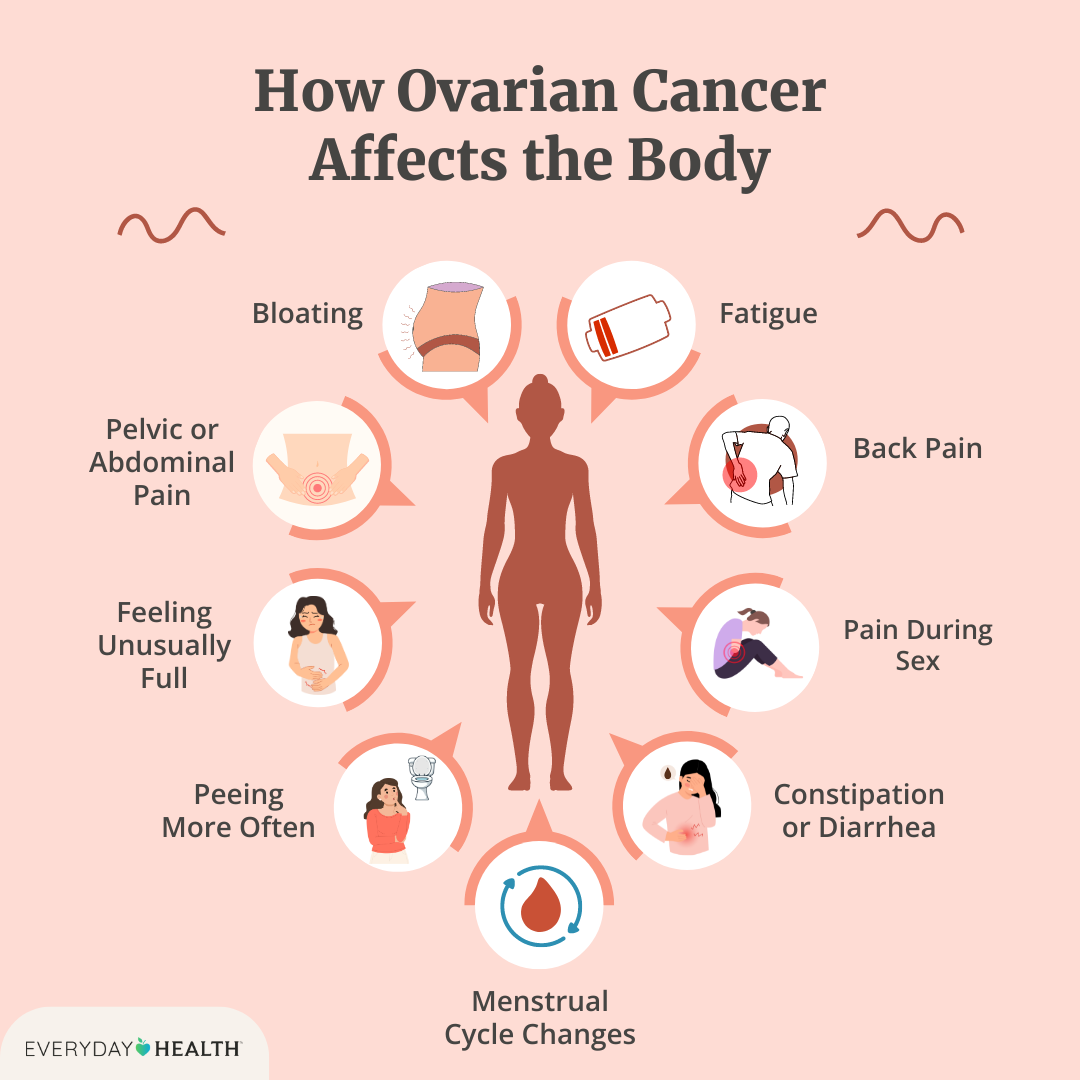
– Symptoms of endometrial cancer include vaginal bleeding after menopause, bleeding between periods, and pelvic pain.
– The cause of endometrial cancer is not known, but it is believed that changes in the DNA of cells in the endometrium lead to the growth of cancer cells.
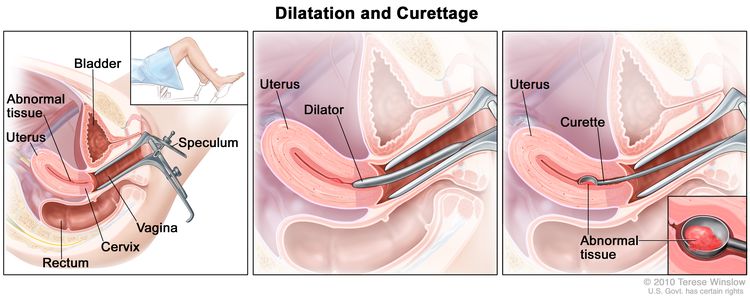
– Early detection of endometrial cancer can lead to successful treatment through surgical removal of the uterus.
– Risk factors for endometrial cancer include changes in hormone balance, certain diseases or conditions, menstruation history, pregnancy history, age, obesity, hormone therapy for breast cancer, and Lynch syndrome.
– Obesity and hormone therapy are notable risk factors for endometrial cancer.
– Lynch syndrome, a genetic syndrome associated with an increased risk of several types of cancer, increases the risk of endometrial cancer.
– Individuals with Lynch syndrome should inquire about appropriate cancer screenings.
– There are no specific facts, stats, or figures provided about endometrioid tumors or the prevalence of Lynch syndrome in the article.
Continue Reading