Have you ever heard of residual ovary syndrome?
It’s a fascinating but often overlooked condition that arises from incomplete removal of ovaries during a surgical procedure called oophorectomy.
Imagine going through a surgery to alleviate your pain, only to discover that you’re still facing discomfort due to cyst formation in your leftover ovary.
In this article, we will delve into the world of residual ovary syndrome and explore the various treatment options available.
Get ready to uncover the mysteries surrounding this intriguing condition!
residual ovary syndrome
Residual ovary syndrome is a condition that occurs when pieces of ovarian tissue are left behind after oophorectomy, the surgical removal of one or both ovaries.
This can happen due to incomplete removal during surgery, and patients with a history of endometriosis or pelvic adhesions are at higher risk.
Symptoms of residual ovary syndrome include irregular menstrual cycles, cyclic pelvic pain, and the formation of pelvic masses.
Diagnosis is done through ultrasound or surgical exploration, and treatment involves surgery to remove the residual tissue and hormonal therapy.
Preventive measures include early treatment of endometriosis and skilled surgery.
Regular follow-ups are recommended after oophorectomy to prevent the development of residual ovary syndrome.
Key Points:
- Residual ovary syndrome occurs when pieces of ovarian tissue are left behind after oophorectomy
- Patients with a history of endometriosis or pelvic adhesions are at higher risk
- Symptoms include irregular menstrual cycles, pelvic pain, and pelvic masses
- Diagnosis is done through ultrasound or surgical exploration
- Treatment involves surgery to remove residual tissue and hormonal therapy
- Preventive measures include early treatment of endometriosis and skilled surgery.
residual ovary syndrome – Watch Video
https://www.youtube.com/watch?v=DnIKnfcJUYc
💡
Pro Tips:
1. Residual Ovary Syndrome trivia: Did you know that residual ovary syndrome, also known as accessory ovary syndrome, refers to a rare condition where fragments of the ovary are left behind after surgical removal?
2. Did you know that residual ovary syndrome can occur when a surgeon inadvertently leaves behind small portions of ovarian tissue during an oophorectomy (surgical removal of the ovaries)?
3. Residual ovary syndrome trivia: In some cases, the residual ovarian tissue left behind after surgery may still have the ability to produce hormones, potentially leading to hormonal imbalances or localized symptoms.
4. Although residual ovary syndrome is a rare condition, some studies suggest that women who have undergone multiple surgeries in the same area may be at a slightly higher risk of developing this syndrome.
5. Interesting fact: Residual ovary syndrome is often difficult to diagnose since its symptoms can mimic other gynecological conditions. It is crucial for doctors to consider this rare syndrome as a potential cause to ensure accurate diagnosis and appropriate treatment.
Oophorectomy: Surgical Removal Of Ovaries
Oophorectomy, also known as ovarian removal surgery, is a medical procedure involving the complete or partial removal of one or both ovaries. It is commonly performed to treat conditions such as pelvic inflammatory disease, endometriosis, chronic pelvic pain, ectopic pregnancy, benign tumors, and large ovarian cysts.
Additionally, oophorectomy may be recommended for women who have BRCA1 or BRCA2 gene mutations in order to reduce the risk of ovarian cancer.
The surgical procedure can be carried out through various approaches, including laparoscopic surgery or traditional open surgery. The choice of method depends on factors such as the patient’s specific condition, the surgeon’s preference, and the available resources.
During the surgery, the goal is to completely remove the affected ovary or ovaries, ensuring no residual ovarian tissue is left behind. However, in some cases, a condition known as residual ovary syndrome may occur.
Reasons For Oophorectomy
Oophorectomy is a surgical procedure performed for various medical conditions. It is aimed at addressing specific issues and providing effective treatment options. Here are some reasons why oophorectomy may be performed:
- Pelvic Inflammatory Disease (PID): Oophorectomy may be necessary to treat PID, which is characterized by inflammation and infection in the female reproductive organs.
- Endometriosis: Oophorectomy can be an effective treatment option for endometriosis, a condition where the tissue lining the uterus grows outside of it, leading to pain and complications.
- Chronic Pelvic Pain: If chronic pelvic pain does not respond to other treatments, the removal of the ovaries may be warranted.
- Ectopic Pregnancy: In cases of ectopic pregnancy, where the fertilized egg implants outside of the uterus, oophorectomy may be necessary to remove the affected ovary.
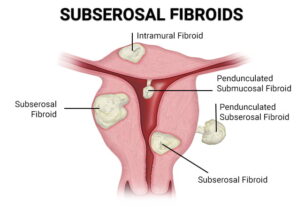
- Benign Tumors and Ovarian Cysts: Surgical intervention, which may involve the removal of the entire ovary, may be required to treat benign tumors and large ovarian cysts.
- Prophylactic Oophorectomy: Women with a high risk of developing ovarian cancer due to mutations in the BRCA1 or BRCA2 genes may be advised to undergo prophylactic oophorectomy. This procedure helps reduce the chances of developing this life-threatening disease.
Remember, oophorectomy is a specialized surgical procedure performed for specific medical reasons under professional medical advice and supervision.
Lowering Ovarian Cancer Risk Through Oophorectomy
One significant benefit of oophorectomy is its potential to significantly lower the risk of ovarian cancer in women with known genetic mutations. The BRCA1 and BRCA2 genes are linked to an increased susceptibility for developing certain types of cancer, including ovarian cancer. By removing the ovaries, which are the primary site of ovarian cancer development, the risk of developing this disease can be reduced.
It’s important to note that oophorectomy is not a guaranteed safeguard against ovarian cancer, as other sites within the body can still develop tumors. However, by removing the ovaries, the risk is significantly diminished in women with specific genetic mutations. This preventive measure is often recommended by healthcare professionals who specialize in cancer genetics and can provide guidance on the most appropriate course of action.
Benefits of Oophorectomy for Lowering Ovarian Cancer Risk:
- Significantly decreases the risk of ovarian cancer in women with genetic mutations
- Removal of ovaries reduces the primary site of ovarian cancer development
“Oophorectomy is a preventive measure recommended by healthcare professionals specializing in cancer genetics to lower the risk of ovarian cancer in women with specific genetic mutations.”
What Is Residual Ovary Syndrome?
Residual ovary syndrome is a condition that occurs when pieces of ovarian tissue are inadvertently left behind in the body after oophorectomy. These remnants of ovarian tissue can implant themselves in the abdominal cavity, leading to complications. If not treated, the residual tissue can cause pain and develop into cysts, which can result in discomfort and potential health issues.
The risk of developing residual ovary syndrome is higher when the ovarian tissue is not completely removed during surgery. Several reasons can contribute to this, including pelvic adhesions, anatomical variations, or poor surgical techniques. Patients with a history of endometriosis or pelvic adhesions are particularly at risk, as these conditions can complicate the surgical removal process.
It is crucial to recognize the symptoms of residual ovary syndrome and seek medical attention promptly if any concerns arise. Symptoms may include irregular menstrual cycles, cyclic pelvic pain, the formation of a pelvic mass, painful intercourse, difficulty urinating, and painful bowel movements. Early diagnosis and intervention are essential for effectively addressing residual ovary syndrome.
Complications Of Residual Ovary Syndrome
Residual ovary syndrome can lead to various complications, primarily stemming from the presence of residual ovarian tissue in the abdominal cavity. One of the most common complications is the growth of cysts within the remnants of ovarian tissue. These cysts can cause pain, discomfort, and may require additional interventions for resolution.
Furthermore, the presence of residual ovarian tissue can result in reimplantation of the tissue on other organs within the abdominal cavity. This can lead to significant pain and interfere with the normal functioning of organs such as the ureters, bowel, and bladder. The complications of residual ovary syndrome can have a significant impact on a person’s quality of life and may require further surgical interventions or ongoing medical management.
It’s crucial for individuals who have undergone oophorectomy to be aware of the potential for residual ovary syndrome and to seek regular follow-up care with their healthcare provider to monitor for any potential complications. Early detection and appropriate treatment can help prevent or alleviate the long-term effects associated with this syndrome.
Factors Increasing Risk Of Residual Ovary Syndrome
Several factors can increase the risk of residual ovary syndrome, particularly in cases where the complete removal of the ovarian tissue is not achieved during oophorectomy. The presence of adhesions within the pelvic region can make it challenging to remove all ovarian tissue accurately. Additionally, anatomical variations in the patient’s reproductive organs can pose challenges during the surgery, potentially leaving behind residual ovarian tissue.
Furthermore, the surgical technique employed can also play a role in determining whether complete removal is achieved. Poor surgical procedures or inadequate skills can increase the likelihood of leaving behind remnants of ovarian tissue. It’s essential for surgeons to have the necessary expertise to perform oophorectomy accurately and remove all ovarian tissue to minimize the risk of residual ovary syndrome.
Patients with a previous history of endometriosis or pelvic adhesions are at a higher risk for developing residual ovary syndrome due to the complexities involved in surgically removing all ovarian tissue. It is crucial for healthcare providers to be aware of these risk factors and to take appropriate precautions during the oophorectomy procedure to minimize the occurrence of this syndrome.
- Factors that increase the risk of residual ovary syndrome:
- Presence of adhesions within the pelvic region
- Anatomical variations in the patient’s reproductive organs
- Poor surgical techniques or inadequate skills
“Patients with a history of endometriosis or pelvic adhesions are at a higher risk for developing residual ovary syndrome. Healthcare providers should be aware of these risk factors and take appropriate precautions during the oophorectomy procedure.”
Symptoms Of Residual Ovary Syndrome
Recognizing the symptoms of residual ovary syndrome is crucial for early detection and effective treatment. The presence of residual ovarian tissue can result in various symptoms that can significantly impact an individual’s quality of life. These symptoms may include:
- Irregular menstrual cycles: occur due to the presence of residual ovarian tissue, which may continue to produce hormones and interfere with the normal hormonal regulation of the menstrual cycle.
- Cyclic pelvic pain: occurring at specific times during the menstrual cycle, can be indicative of residual ovary syndrome.
- Formation of a pelvic mass: can also be observed, resulting from the growth or cystic changes within the remnants of ovarian tissue.
Additionally, individuals with residual ovary syndrome may experience:
- Painful intercourse (dyspareunia): due to the presence of residual ovarian tissue in close proximity to the reproductive organs, leading to discomfort during sexual activity.
- Difficulty in urination: tissue remnants may impact the normal functioning of the bladder.
- Painful bowel movements: tissue remnants may also impact the normal functioning of the bowel.
It is essential for individuals who have undergone oophorectomy to be vigilant about any changes or symptoms they experience and to promptly consult with their healthcare provider if any concerns arise. Early diagnosis and appropriate treatment can help alleviate the symptoms associated with residual ovary syndrome.
Diagnosis Of Residual Ovary Syndrome
The diagnosis of residual ovary syndrome involves various techniques to identify the presence of residual ovarian tissue and assess its impact on an individual’s health.
One of the primary diagnostic tools is a pelvic ultrasound, which uses sound waves to create images of the pelvic region. This imaging modality can provide valuable information about:
- The presence of ovarian tissue remnants
- The presence of cysts
- Abnormalities within the pelvic region
In cases where ultrasound imaging is inconclusive or further information is required, surgical exploration and biopsy of the remnant ovarian tissue may be performed. This involves a more invasive approach and is typically carried out via laparoscopy.
During laparoscopic exploration:
- A small incision is made in the abdomen
- A laparoscope is inserted to visualize the pelvic region
- Residual ovarian tissue is located
- A biopsy sample is obtained for further analysis
The combination of these diagnostic techniques can help healthcare providers confirm the presence of residual ovary syndrome and determine the appropriate course of treatment.
“Accurate diagnosis is crucial to ensure that individuals receive the necessary interventions to address any symptoms or complications associated with this syndrome.”
Treatment Options For Residual Ovary Syndrome
The treatment of residual ovary syndrome typically involves a combination of surgical intervention and hormonal therapy to address the presence of residual ovarian tissue and manage resulting symptoms. The primary goal of treatment is the complete removal of the residual ovarian tissue to alleviate any pain or complications.
- Surgical removal of the residual ovarian tissue can be performed via laparoscopic surgery, similar to the initial oophorectomy procedure. Through small incisions, the surgeon can locate and remove the remnants of ovarian tissue, minimizing the risk of recurrence or complications. This surgical approach is generally less invasive and associated with shorter recovery times compared to traditional open surgery.
- In addition to surgical removal, hormonal therapy may be recommended to manage symptoms and regulate any residual hormonal production. Hormonal therapy may involve the use of medications such as birth control pills or hormone replacement therapy to provide hormonal balance and alleviate associated symptoms such as irregular menstrual cycles or pelvic pain.
It’s important for individuals with residual ovary syndrome to work closely with their healthcare provider to develop a treatment plan that addresses their specific needs and concerns. Regular follow-up appointments are advised to monitor the effectiveness of treatment and ensure optimal management of this condition.
- Surgical intervention and hormonal therapy are the primary treatment options for residual ovary syndrome.
- Surgical removal of residual ovarian tissue is typically done through laparoscopic surgery for reduced invasiveness and quicker recovery.
- Hormonal therapy, involving the use of birth control pills or hormone replacement therapy, can help manage symptoms and regulate hormonal production.
- Consulting with a healthcare provider and scheduling regular follow-up appointments is crucial for effective management of residual ovary syndrome.
Preventive Measures And Follow-Up Care For Oophorectomy
To reduce the risk of developing residual ovary syndrome, there are several preventive measures that can be taken before and during the oophorectomy procedure. Early surgical treatment of conditions such as endometriosis, which may require the removal of the ovaries, can help minimize the risk of complications and the need for additional procedures. It is crucial for women with known endometriosis to work closely with their healthcare provider to explore appropriate treatment options and interventions to manage this condition effectively.
Skilled surgery for ovary removal is essential to ensure complete removal of the ovarian tissue and minimize the risk of residual ovary syndrome. Surgeons specializing in gynecological procedures should have the necessary expertise and experience to perform oophorectomy accurately. It is recommended to seek opinion from a specialist in cases of complex conditions or when there are concerns about the surgical procedure.
Following oophorectomy, regular follow-up care with a healthcare provider is crucial to monitor for any signs or symptoms of residual ovary syndrome. Routine check-ups can help detect any complications early and ensure that appropriate interventions are initiated as necessary. Patients should openly communicate any concerns or changes they observe, as early intervention can often lead to better outcomes.
In conclusion, oophorectomy is a surgical procedure involving the removal of one or both ovaries. This procedure is performed for various reasons, including the treatment of conditions such as endometriosis, pelvic inflammatory disease, and large ovarian cysts. Oophorectomy can also be undertaken to reduce the risk of ovarian cancer in individuals with known BRCA1 or BRCA2 gene mutations.
Despite the benefits of oophorectomy, residual ovary syndrome can occur when pieces of ovarian tissue are left behind after surgery. This condition can lead to complications such as the development of cysts and reimplantation of tissue on other organs within the abdominal cavity. Recognition of the symptoms and timely diagnosis of residual ovary syndrome is crucial for appropriate management and treatment.
Various treatment options are available for residual ovary syndrome, including surgical removal of the residual ovarian tissue and hormonal therapy. Preventive measures, such as early treatment of endometriosis and skilled surgery, can help minimize the risk of developing this syndrome. Regular follow-up care with a healthcare provider is essential to monitor for any potential complications and ensure optimal management of individuals who have undergone oophorectomy.
💡
You may need to know these questions about residual ovary syndrome
What are the symptoms of residual ovarian syndrome?
Residual ovarian syndrome (ROS) is characterized by various symptoms that can occur following a hysterectomy. The most common indicators include pelvic pain, pelvic mass, and dyspareunia, either experienced individually or in combination. Roughly 5% of patients who undergo hysterectomy are estimated to develop ROS, necessitating surgical intervention to alleviate the symptoms and address the underlying pathology in the conserved ovaries. These symptoms serve as warning signs to consider the possibility of ROS and take appropriate measures for diagnosis and treatment.
How do you treat residual ovarian syndrome?
The management of residual ovarian syndrome primarily involves surgical intervention to remove any remaining ovarian tissue. This procedure aims to alleviate the symptoms and prevent further complications. In cases where there is a pelvic mass, a thorough evaluation should be conducted to rule out any potential malignancy. If surgery is not suitable or the patient declines, hormonal therapy can be considered as an alternative approach to suppress ovarian function and mitigate the impact of the syndrome. However, it is crucial to seek medical advice for personalized treatment recommendations and the best course of action.
How do you treat a residual ovarian cyst?
Treatment for a residual ovarian cyst typically involves surgical removal of the remaining ovarian tissue. It is crucial to evaluate the patient for malignancy if they have a pelvic mass along with the cyst. In cases where surgery is not possible or the patient refuses it, hormonal therapy may be considered to suppress ovarian function as an alternative treatment method.
Is ovarian remnant syndrome serious?
Ovarian remnant syndrome can range in seriousness depending on the individual case. While some cases may not present any noticeable symptoms and can be left untreated without significant consequences, other cases of untreated ORS can lead to the continued growth of cysts, resulting in more severe pelvic pain. Therefore, it is important to monitor and address symptoms to prevent potential complications and alleviate discomfort.
Reference source
https://www.sciencedirect.com/science/article/pii/S1028455918301943
https://pubmed.ncbi.nlm.nih.gov/9890231/
https://en.wikipedia.org/wiki/Ovarian_remnant_syndrome
https://www.icliniq.com/articles/womens-health/residual-ovary-syndrome