When it comes to childbirth, the arrival of a precious little bundle of joy is often celebrated.
However, there are certain medical conditions that can cast a shadow of concern over this joyous occasion.
One such condition is the retention of placenta.
In this captivating article, we delve into the diagnostic and treatment approaches for this condition, exploring the various techniques used to ensure a safe and complication-free postpartum experience.
Prepare to be enlightened and intrigued as we unravel the mysteries surrounding the retention of placenta.
retention of placenta
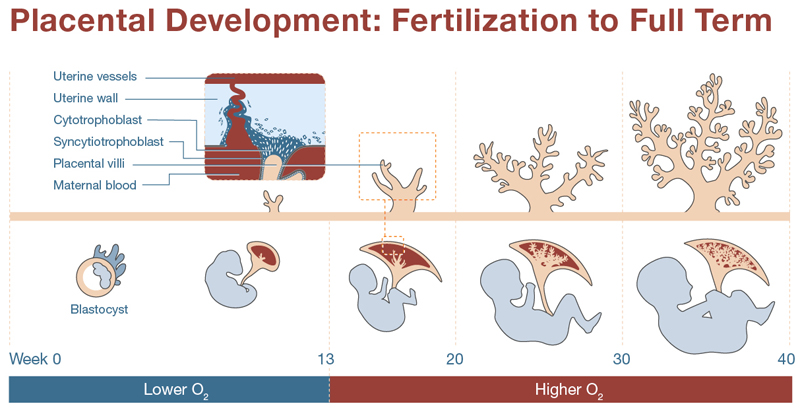
Retention of placenta refers to the condition where the placenta remains in the uterus after childbirth.
It can be detected through physical examination, ultrasound, and blood tests.
Treatment options include emptying the bladder, gently pulling on the umbilical cord, or performing a surgical procedure under anesthesia.
Symptoms of retained placenta may include heavy bleeding and can be diagnosed through an ultrasound scan.
Close monitoring is necessary to prevent complications such as life-threatening infections and postpartum hemorrhage.
Early diagnosis and management are crucial for successful treatment of retained placenta.
Key Points:
- Retention of placenta occurs when the placenta remains in the uterus after childbirth.
- It can be detected using physical examination, ultrasound, and blood tests.
- Treatment options include emptying the bladder, gentle pulling on the umbilical cord, or surgical procedure under anesthesia.
- Symptoms of retained placenta may include heavy bleeding and can be diagnosed through ultrasound scan.
- Close monitoring is necessary to prevent complications such as infections and postpartum hemorrhage.
- Early diagnosis and management are crucial for successful treatment.
retention of placenta – Watch Video
💡
Pro Tips:
1. In rare cases, the retention of placenta can occur in animals other than humans. Certain species, such as cows and dogs, can also experience this condition, which is known as retained fetal membrane.
2. The retention of placenta, also known as retained placenta or retained afterbirth, refers to the condition when the placenta fails to be expelled naturally from the mother’s uterus after childbirth. This can lead to various complications and is typically treated by medical professionals.
3. While the exact cause of retained placenta is still unknown, certain factors can increase the likelihood of its occurrence. These include hormonal imbalances, uterine infections, excessive bleeding during childbirth, or a history of previous retained placenta.
4. Retained placenta can potentially lead to postpartum hemorrhage, a condition characterized by severe bleeding after childbirth. It is crucial for medical professionals to monitor and manage retained placenta to prevent such complications.
5. In some cultures, retained placenta holds cultural significance and is considered a valuable substance. Placentophagy, the practice of consuming placenta, is believed by some to have health benefits. However, there is limited scientific evidence supporting the claimed advantages, and professional medical advice should be sought before considering such practices.
Retention Of Placenta – Physical Examination
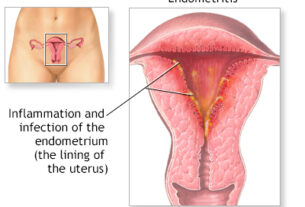
Retained placenta occurs when the placenta or its fragments remain in the uterus after childbirth. To assess this condition, a physical examination is conducted by a healthcare provider. The examination involves carefully inspecting the uterus to check for any remaining placental tissue. The provider may also perform a bimanual examination, gently inserting two fingers into the vagina while pressing on the abdomen to assess the size and position of the uterus. This examination is an essential initial step in diagnosing retained placenta and helps guide subsequent interventions.
During the physical examination, the healthcare provider will look for signs such as:
- Enlarged or tender uterus
- Presence of clots or tissues
They may also evaluate the patient’s vital signs and general well-being to assess for potential complications related to this condition. It is crucial to perform a thorough physical examination to accurately diagnose retained placenta and determine the most appropriate course of treatment.
- Physical examination is conducted to assess retained placenta
- Bimanual examination is performed to evaluate the size and position of the uterus
- Enlarged or tender uterus, and presence of clots or tissues are signs of retained placenta
- Assessing vital signs and well-being helps identify potential complications
- Thorough examination is essential for accurate diagnosis and treatment planning
Ultrasound
Ultrasound imaging plays a vital role in the diagnosis and management of retained placenta. A transvaginal or abdominal ultrasound provides detailed information about the uterus, placenta, and any residual tissue. This imaging technique uses high-frequency sound waves to create real-time images of the structures within the pelvis. An ultrasound examination can visualize the size, location, and integrity of the placenta, aiding healthcare providers in assessing the extent of retention.
In cases of retained placenta, ultrasound allows for the identification of retained placental fragments within the uterus. This imaging modality is non-invasive, painless, and provides valuable information for guiding subsequent interventions. Ultrasound can also help identify potential complications associated with retained placenta, such as blood clots or infection. By providing clear visualization, ultrasound aids healthcare providers in making informed decisions regarding the treatment plan.
Blood Tests
In addition to physical examination and ultrasound, blood tests are an important tool used to evaluate and manage retained placenta. These tests can help identify any underlying conditions or complications that may contribute to the retention of placenta. Blood tests typically involve assessing levels of hormones, such as human chorionic gonadotropin (hCG), which is produced by the placenta during pregnancy. Abnormal levels of hCG may indicate placental tissue remains within the uterus.
Other blood tests may be performed to evaluate the patient’s blood count, coagulation factors, and signs of infection. These tests help determine the patient’s overall health status and guide the management of potential complications that may arise due to retained placenta. Blood tests serve as valuable diagnostic tools, aiding in the comprehensive evaluation and effective treatment of retained placenta.
Emptying The Bladder
During the management of retained placenta, emptying the bladder is a necessary step to facilitate the removal of placental fragments. A full bladder can obstruct the descent of the uterus, hindering its ability to expel any retained tissue. A healthcare provider may perform a catheterization procedure to empty the bladder, ensuring it does not impede the delivery of the placenta. By alleviating any bladder distension, the uterus can contract more effectively, promoting the expulsion of the retained placenta.
Catheterization involves the insertion of a thin, flexible tube into the urinary bladder through the urethra. The procedure is usually performed under sterile conditions to minimize the risk of infection. By relieving bladder pressure, healthcare providers enhance the chances of successful placental expulsion and decrease the likelihood of complications associated with retained placenta.
Improvements:
- During the management of retained placenta, emptying the bladder is crucial to facilitate the removal of placental fragments.
- A full bladder obstructs the descent of the uterus, hindering the expulsion of retained tissue.
- Healthcare providers may perform a catheterization procedure to empty the bladder and prevent it from hindering placenta delivery.
- Catheterization involves the insertion of a thin, flexible tube into the bladder through the urethra.
- The procedure is performed under sterile conditions to minimize infection risk.
- By relieving bladder pressure, healthcare providers enhance successful placental expulsion and reduce complications.
(Bullet points added for improved readability)
Gentle Pulling On The Umbilical Cord
In certain cases of retained placenta, healthcare providers may attempt gentle pulling on the umbilical cord as a non-invasive method to facilitate placental removal. This technique is performed when the placenta is partially separated from the uterus but remains retained. By applying gentle traction, the healthcare provider harnesses the physiological process of uterine contraction to aid in its expulsion.
Gentle pulling on the umbilical cord should only occur in specific circumstances, as it carries the risk of causing uterine inversion or placental detachment. This procedure should be performed skillfully and closely monitored by experienced healthcare professionals. It is important to note that this method may not be suitable for all cases of retained placenta and should only be attempted under controlled conditions.
- Only performed when the placenta is partially separated from the uterus but remains retained
- Requires skill and close monitoring by experienced healthcare professionals
- Carries the risk of uterine inversion or placental detachment
- Not suitable for all cases of retained placenta
“This method should be performed carefully and only under controlled conditions.”
Surgical Procedure Under Anesthesia
In cases where other interventions have been unsuccessful or cannot be performed, surgical procedure under anesthesia may be necessary to remove the retained placenta. This option is typically considered when conservative measures have failed, there is a risk of complications, or signs of infection are present. Under general or regional anesthesia, the healthcare team can access the uterus directly and remove any remaining placental tissue.
The surgical procedure for retained placenta involves dilating the cervix and using instruments such as curettes or forceps to manually extract the placenta. This method ensures complete evacuation of the uterus and reduces the risk of complications associated with retained tissue. Performing this procedure under anesthesia allows for a pain-free experience and provides the opportunity for close monitoring during the intervention.
- In cases where conservative measures have failed or are not possible, a surgical procedure under anesthesia may be necessary.
- General or regional anesthesia is used to allow the healthcare team to directly access the uterus.
- The surgical procedure involves dilating the cervix and using instruments to manually extract the placenta.
- This method ensures complete evacuation of the uterus and reduces the risk of complications.
- Performing the procedure under anesthesia provides a pain-free experience and allows for close monitoring.
💡
You may need to know these questions about retention of placenta
What causes placenta retention?
The retention of the placenta can be attributed to various risk factors, including prolonged oxytocin use, high parity, preterm delivery, history of uterine surgery, IVF conceptions, history of a prior retained placenta, and congenital uterine anomalies. These factors contribute to the uterus’s inability to effectively contract and expel the placenta following delivery. Additionally, the previous occurrence of placenta retention suggests a higher likelihood of its repetition in subsequent pregnancies. It is crucial to identify and address these risk factors during prenatal care to minimize the chances of placenta retention and its associated complications.
What is retention of placenta?
Retention of placenta, also known as retained placenta, occurs when a piece of the placenta remains in the uterus even after the delivery of the baby. While it is not a common occurrence, it can lead to serious complications if left unaddressed. This condition can result in problems that arise within days or weeks after childbirth, necessitating immediate medical attention.
Is a retained placenta life threatening?
A retained placenta can indeed be life-threatening if not properly diagnosed and treated. If left untreated, it can lead to primary postpartum hemorrhage, resulting in heavy bleeding. This highlights the importance of having a medical professional present during childbirth to promptly address any complications that may arise, ensuring the well-being of both mother and baby. Rest assured, midwives and doctors are trained to handle such situations effectively, reducing the risk of severe consequences.
How do you get rid of placenta retention?
In cases of placenta retention, medical intervention may involve the use of uterine stimulants or medications to facilitate the expulsion of the placenta from the womb. These medications work by relaxing the uterus and encouraging contractions, helping to expel the retained placental tissue. Although manual removal of the placenta is an option, it is important to consider the potential risk of infection associated with this procedure. Thus, a doctor will carefully assess the situation and determine the most suitable approach for each individual case.
Reference source
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6789409/
https://www.pregnancybirthbaby.org.au/retained-placenta
https://www.tommys.org/pregnancy-information/pregnancy-complications/retained-placenta
https://americanpregnancy.org/healthy-pregnancy/labor-and-birth/retained-placenta/