Placental abruption, an enigma hidden within the depths of the womb, silently threatens the delicate bond between mother and child.
Like a clandestine force, it strikes with unexpected fury, unleashing a torrent of blood.
In this gripping tale of life and death, we delve into the mysteries of diagnosis, risk factors, and management, as the truth of this devastating condition is artfully revealed.
Brace yourself for a revelation unlike any other, as we uncover the secrets of placental abruption.
revealed abruption
Revealed abruption is a type of placental abruption characterized by visible vaginal bleeding.
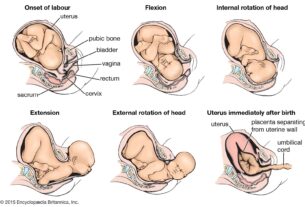
Placental abruption occurs when part or all of the placenta separates from the uterus prematurely.
Major risk factors for placental abruption include previous abruption, pre-eclampsia, abnormal lie of the baby, abdominal trauma, smoking or drug use, bleeding in the first trimester, and underlying thrombophilias.
Clinical features of placental abruption include painful vaginal bleeding, woody and painful uterus on palpation, and the need for systematic assessment and resuscitation.
Diagnosis can be made through general examination, including assessing pallor, distress, peripheral circulation, abdominal tenderness, and the lie and presentation of the fetus.
Investigations such as hematological and biochemical tests, fetal wellbeing assessment, and ultrasound scan should also be performed.
Management depends on the severity and fetal health, ranging from emergency delivery to conservative management.
Placental abruption complicates approximately 1% of pregnancies and increases the risk of maternal, fetal, and neonatal morbidity and mortality.
Risk factors include smoking, substance abuse, maternal age, hypertension, and previous abruption.
Trauma and radiological imaging, such as ultrasound and CT scans, can aid in diagnosing placental abruption.
Key Points:
- Revealed abruption is characterized by visible vaginal bleeding and occurs when part or all of the placenta separates from the uterus prematurely.
- Major risk factors for placental abruption include previous abruption, pre-eclampsia, abnormal lie of the baby, abdominal trauma, smoking or drug use, bleeding in the first trimester, and underlying thrombophilias.
- Clinical features of placental abruption include painful vaginal bleeding, woody and painful uterus, and the need for systematic assessment and resuscitation.
- Diagnosis can be made through general examination, including assessing pallor, distress, peripheral circulation, abdominal tenderness, and the lie and presentation of the fetus.
- Investigations such as hematological and biochemical tests, fetal wellbeing assessment, and ultrasound scan should be performed.
- Management of placental abruption depends on severity and fetal health, ranging from emergency delivery to conservative management.
revealed abruption – Watch Video
https://www.youtube.com/watch?v=0yUORSHifKM
💡
Pro Tips:
1. The Grand Canyon’s revealed abruption showcases nearly two billion years of Earth’s geological history, unveiling layers dating back to the Precambrian era.
2. The discovery of a fossilized tree trunk within the revealed abruption of Antarctica confirmed that the continent once hosted lush forests during the prehistoric era.
3. The revealed abruption of a lost underwater city off the coast of India astonished archaeologists, revealing evidence of an ancient civilization dating back over 9,000 years.
4. When the revealed abruption of a hidden cave in France was explored, researchers discovered prehistoric paintings that are believed to be over 30,000 years old, making them some of the oldest known artworks in the world.
5. A recently revealed abruption on the surface of the Moon has provided scientists with new insights into lunar geology, leading to the discovery of valuable resources such as water ice, which could potentially support future lunar missions.
Types Of Placental Abruption: Revealed Vs. Concealed
Placental abruption is a serious complication during pregnancy where a part or all of the placenta separates from the uterus prematurely, resulting in vaginal bleeding. There are two main types of placental abruption: revealed and concealed.
Revealed abruption is characterized by visible vaginal bleeding. Women with this type of abruption often experience significant blood loss and may notice blood clots or tissue passing through the vagina. The bleeding can range from mild to severe and may be accompanied by abdominal pain or cramping. It is important for women experiencing revealed abruption to seek immediate medical attention as this condition can be life-threatening if not properly managed.
On the other hand, concealed abruption involves bleeding that remains within the uterus and may not be visible externally. The blood trapped behind the placenta can pool, causing the uterus to enlarge and become tense and tender. This type of abruption can be more difficult to diagnose as there may be no external signs of bleeding. However, it is equally important to recognize and treat concealed abruption promptly as it can also have serious consequences for both the mother and fetus.
Risk Factors For Placental Abruption
Several risk factors have been identified for placental abruption. Previous placental abruption is one of the major risk factors, as women who have experienced it in a previous pregnancy have an increased likelihood of experiencing it again. Other risk factors include pre-eclampsia, a condition characterized by high blood pressure and damage to organs such as the liver and kidneys; abnormal lie of the baby, where the baby is not in the optimal position for delivery; abdominal trauma, such as from a fall or car accident; smoking or drug use, which can increase the risk of placental problems; bleeding in the first trimester; and underlying thrombophilias, which are blood clotting disorders.
It is important for women with these risk factors to receive appropriate antenatal care and be closely monitored throughout their pregnancy to detect any signs of placental abruption early on.
Clinical Features Of Placental Abruption
When a placental abruption occurs, there are several clinical features that may be observed. The most common symptom is painful vaginal bleeding, which can range from light spotting to heavy bleeding. Abdominal pain or cramping is also common, varying in intensity.
On physical examination, the uterus may feel woody and painful to touch, indicating a significant abruption that may require immediate intervention. Systematic assessment and resuscitation are essential for managing placental abruption, as both the mother and baby can be at risk of complications.
Other clinical features to be aware of include:
- Pale skin suggesting anemia
- Signs of distress in the mother
- Changes in peripheral circulation
- Abdominal tenderness
It is also important to assess the position and presentation of the fetus/fetuses, as this can have implications for the management of the abruption.
General Examination And Assessment Of Bleeding During Pregnancy
When assessing bleeding during pregnancy, a thorough general examination is essential to determine the cause and severity of the bleeding. This examination involves assessing the woman for signs of pallor, distress, and peripheral circulation. Abdominal tenderness should also be evaluated, as this can indicate a potential placental abruption.
In addition, the feel of the uterus should be assessed through palpation. A woody and painful uterus may suggest a significant abruption and should prompt further investigation and management.
To gather more information, it is important to review the woman’s hand-held pregnancy notes for scan reports. This can help identify any potential issues with the placenta, such as placenta praevia, which can sometimes present with bleeding.
When assessing the bleeding externally, it is important to examine the woman’s pads for any signs of blood loss. Speculum examination should be avoided until placenta praevia has been excluded, as this can cause further bleeding. Taking triple genital swabs can also help exclude any potential infection, which can sometimes present with bleeding.
It is crucial to exercise caution when performing a digital vaginal examination, especially in cases of known placenta praevia, as this can lead to significant bleeding.
By conducting a thorough general examination and assessment, healthcare professionals can gather valuable information to help determine the cause and severity of the bleeding during pregnancy, allowing for appropriate and timely management.
Placental Abruption As A Cause Of Antepartum Hemorrhage
Antepartum hemorrhage refers to bleeding that occurs after 24 weeks of gestation but before the onset of labor. Placental abruption is a common cause of antepartum hemorrhage and should be considered in any pregnant woman presenting with vaginal bleeding during this time.
Placental abruption can result in varying degrees of bleeding, ranging from mild to severe. The severity of the bleeding depends on the extent of the placental separation and the amount of blood accumulating behind the placenta. Severe cases of placental abruption can lead to significant maternal and fetal morbidity and mortality if not managed promptly.
It is crucial for healthcare professionals to recognize the signs and symptoms of placental abruption and initiate appropriate management to ensure the best possible outcomes for both the mother and baby.
Investigations For Placental Abruption
When placental abruption is suspected, several investigations should be performed to confirm the diagnosis and assess the extent of the condition. These investigations aim to evaluate the maternal and fetal well-being and guide further management decisions.
Hematology tests, such as a full blood count and Kleihauer test, help assess the mother’s blood count and determine the presence of fetal blood in the maternal circulation, respectively. Group and save and cross-match tests are essential to ensure that blood products are readily available if the mother requires transfusion.
Biochemistry tests, including urea and electrolytes and liver function tests, provide valuable information about the mother’s general health and organ function.
Fetal well-being assessment, often performed through a cardiotocograph (CTG), helps monitor the baby’s heart rate and uterine contractions to ensure adequate oxygen supply.
These investigations collectively contribute to the overall assessment of the condition and help guide management decisions to optimize maternal and fetal outcomes.
Role Of Ultrasound In Assessing Placental Abruption
Ultrasound scanning plays a crucial role in the assessment of placental abruption. It allows healthcare professionals to visualize the placenta, evaluate its position and integrity, and assess the extent of separation.
Ultrasound scans should be performed when placental abruption is suspected. However, it is important to note that ultrasound alone cannot definitively exclude the presence of abruption, especially in cases where there may be concealed bleeding.
Despite this limitation, ultrasound remains the preferred imaging modality for assessing placental abruption due to its benefits of avoiding ionizing radiation, allowing for dynamic real-time imaging, and its widespread availability.
It is essential for healthcare professionals to be trained in the interpretation of ultrasound scans for placental abruption to ensure accurate diagnosis and appropriate management.
Management Options For Placental Abruption
The management of placental abruption depends on the health of the fetus and the severity of the abruption. Early identification and prompt intervention are crucial to optimize maternal and fetal outcomes.
In cases where there is evidence of maternal and/or fetal compromise, emergency delivery is indicated. This may involve either cesarean section or, in some cases, assisted vaginal delivery, depending on the clinical situation.
For cases of hemorrhage at term without compromise, induction of labor is recommended. This aims to expedite delivery and reduce the risk of further complications.
Conservative management is an option for some partial or marginal abruptions without maternal or fetal compromise. Close monitoring of the mother and fetus is necessary to detect any signs of deterioration that may require intervention.
The management of placental abruption requires a multidisciplinary approach involving obstetricians, midwives, anesthetists, and neonatologists. Regular assessment of the mother and baby is vital to ensure timely intervention if complications arise.
Anti-D Administration For Rhesus D Negative Women
For women who are rhesus D negative and experience vaginal bleeding associated with placental abruption, administration of Anti-D immunoglobulin within 72 hours of the bleeding onset is recommended. This helps prevent the development of rhesus D sensitization, which can have implications for future pregnancies.
Placental abruption can lead to the mixing of maternal and fetal blood, potentially causing sensitization in women who are rhesus D negative and carrying a rhesus D positive baby. Administration of Anti-D immunoglobulin helps prevent the mother’s immune system from developing antibodies against rhesus D positive blood, reducing the risk of complications in subsequent pregnancies.
It is important for healthcare professionals to be aware of the need for Anti-D administration in these cases and ensure timely and appropriate intervention.
- Bullet point 1: Anti-D immunoglobulin should be administered within 72 hours of the onset of vaginal bleeding associated with placental abruption in women who are rhesus D negative.
- Bullet point 2: This preventive measure helps reduce the risk of rhesus D sensitization and its implications for future pregnancies.
- Bullet point 3: Placental abruption can cause mixing of maternal and fetal blood, leading to potential sensitization in rhesus D negative women carrying a rhesus D positive baby.
- Bullet point 4: Administration of Anti-D immunoglobulin prevents the development of antibodies against rhesus D positive blood in the mother’s immune system.
- Bullet point 5: Healthcare professionals should be aware of the importance of timely and appropriate intervention in these cases.
It is crucial to promptly administer Anti-D immunoglobulin to rhesus D negative women experiencing vaginal bleeding associated with placental abruption to prevent complications in future pregnancies.
Impact And Incidence Of Placental Abruption In Pregnancy
Placental abruption complicates approximately 1% of pregnancies, making it a relatively common occurrence. It poses significant risks to both maternal and fetal health and can result in increased morbidity and mortality.
Risk factors for placental abruption include:
- smoking, alcohol or cocaine use during pregnancy
- advanced maternal age
- history of maternal hypertension and preeclampsia
- previous placental abruption
- multiple gestational pregnancies
Trauma from a motor vehicle accident, fall, or blow to the abdomen can also cause placental abruption. Pregnant women should take appropriate precautions and seek medical attention if they experience any significant impact to the abdominal area.
The use of radiologic imaging, such as ultrasonography, can assist in diagnosing placental abruption. Ultrasonography is usually the preferred study due to its benefits of avoiding ionizing radiation, providing real-time imaging, and being widely available.
In cases of severe trauma, additional imaging such as CT scanning may be required to assess for other abdominopelvic injuries.
The American College of Radiology guidelines recommend ultrasound FAST scans as a limited bedside adjunct for triage in pregnant patients with major blunt trauma. Healthcare professionals should follow these guidelines and make appropriate imaging decisions to ensure the best care for pregnant patients.
In conclusion, placental abruption is a serious complication during pregnancy that can have significant health implications for both the mother and baby. Recognizing the different types of abruption, understanding the risk factors, and being aware of the clinical features are crucial for early diagnosis and appropriate management. Through thorough examination, appropriate investigations, and the use of imaging techniques, healthcare professionals can effectively assess and manage placental abruption to optimize outcomes for both mother and baby.
💡
You may need to know these questions about revealed abruption
What is revealed and concealed Abruptio Placentae?
Abruptio placentae, a serious complication during pregnancy, can manifest in two distinct ways: revealed and concealed. In the revealed type, the separation of the placenta causes bleeding that flows through the cervix, leading to noticeable vaginal bleeding. On the other hand, concealed placental abruption involves the bleeding staying contained within the uterus. Instead of flowing out, the blood typically forms a clot behind the placenta, known as a retroplacental clot. This concealed bleeding is not immediately evident through vaginal bleeding and can be more challenging to diagnose without proper medical monitoring. Consequently, concealed placental abruption poses additional risks and demands heightened awareness during pregnancy.
Can a baby survive a placental abruption?
Survival for a baby facing placental abruption can be challenging due to the potential complications it causes. Placental abruption is a serious condition that poses a risk of prematurity, stillbirth, and hypoxia. With perinatal mortality rates around 10%, it is evident that a baby’s chances of survival may be significantly impacted. Immediate medical attention and extensive neonatal care become critical factors in increasing the likelihood of surviving a placental abruption.
How serious is placental abruption?
Placental abruption is a potentially grave condition that can have severe consequences for both the pregnant woman and her unborn child. While the cause of placental abruption is often unknown, certain risk factors such as maternal high blood pressure, abdominal trauma, and substance misuse can increase the likelihood of this condition. If left untreated, placental abruption can result in devastating outcomes, including fatalities for both the mother and the baby. It is crucial for individuals experiencing symptoms or risk factors associated with placental abruption to seek immediate medical attention to mitigate the potentially dire effects of this condition.
Is Abruptio Placentae an emergency?
Abruptio Placentae, also known as placental abruption, is indeed considered a medical emergency. This condition can occur unexpectedly, leaving little to no time for preparation. In some cases, healthcare providers may be able to identify signs of an impending abruption, and depending on its severity, patients may be admitted to the hospital for close monitoring. The time-sensitive nature of this condition emphasizes the urgency and critical nature of the situation, warranting immediate medical attention.
Reference source
https://emedicine.medscape.com/article/402314-overview
https://teachmeobgyn.com/pregnancy/medical-disorders/placental-abruption/
https://publications.aap.org/pediatrics/article/142/2/e20173915/37549/Placental-Abruption-and-Child-Mortality
https://www.betterhealth.vic.gov.au/health/healthyliving/placental-abruption