When it comes to childbirth, the miracle of life and joyous moments are often at the forefront of our minds.
However, lurking in the shadows is a potential nightmare that could shatter the bliss – a rupture of the uterus.
This terrifying and rare occurrence demands our attention as we delve into the world of a medical mystery with devastating consequences.
Prepare to be captivated by the haunting tales of rupture and the enlightening knowledge that awaits.
rupture of uterus
Rupture of the uterus is a serious medical condition characterized by a tear or rupture in the wall of the uterus.
This condition is usually associated with pregnancy and childbirth and can pose significant risks to both the mother and the baby.
Immediate medical intervention is necessary to manage the situation and prevent further complications.
Key Points:
- Rupture of the uterus is a tear or rupture in the wall of the uterus that can occur during pregnancy or childbirth.
- This condition poses significant risks to both the mother and the baby.
- This is a serious medical condition that requires immediate medical intervention.
- The tear or rupture in the uterus can result in complications if not managed properly.
- Pregnancy and childbirth are usually associated with this condition.
- Prompt medical intervention is crucial to prevent further complications.
rupture of uterus – Watch Video
💡
Pro Tips:
1. The rupture of uterus, also known as uterine rupture, is a rare but potentially life-threatening complication during pregnancy or childbirth.
2. Uterine rupture occurs when there is a tearing or separation of the muscular wall of the uterus. This can result in severe bleeding and can endanger the mother and the baby.
3. Although rare, the risk of uterine rupture is higher in women who have had previous uterine surgeries, such as a cesarean section or other uterine incisions.
4. Uterine rupture can cause intense abdominal pain, abnormal positioning of the baby, a rapid drop in heart rate, and loss of the fetal monitoring signal.
5. Immediate surgical intervention is required to control bleeding and repair the ruptured uterus. In some severe cases, a hysterectomy (removal of the uterus) may be necessary to save the mother’s life.
Definition of Rupture of Uterus
Rupture of the uterus is a severe and potentially life-threatening condition that occurs when there is a tear or a separation in the wall of the uterus. This rupture can happen during pregnancy, labor, or even after delivery. It is considered to be a rare but serious complication that requires immediate medical attention.
When a rupture occurs, the contents of the uterus, including the fetus, can spill into the abdominal cavity, leading to significant maternal and fetal morbidity or mortality.
The severity of a uterine rupture can vary. It can range from a small tear in the uterine wall, known as an incomplete rupture, to a complete rupture where the uterus splits open along its entire length. Incomplete ruptures are usually less severe and can be managed more easily, while complete ruptures require immediate surgical intervention to prevent further complications.
Causes of Rupture of Uterus
Several factors can contribute to the occurrence of a uterine rupture. One of the most common causes is a previous cesarean section scar. Women who have had a previous cesarean delivery are at a higher risk of uterine rupture, especially if they attempt a vaginal birth after cesarean (VBAC).
Other causes include:
- Trauma to the abdomen, such as a car accident or a fall,
- Abnormal attachment of the placenta (placenta previa),
- Prolonged or obstructed labor,
- Improper use of labor-inducing medications, or
- Improper administration of uterine stimulant drugs.
It is important to note that while a rupture can happen during pregnancy, labor, or postpartum, the majority of cases occur during labor and delivery. This is due to the increased pressure within the uterus and the physical stress placed on the uterine wall during contractions.
Improved Text:
Several factors can contribute to the occurrence of a uterine rupture. One of the most common causes is a previous cesarean section scar. Women who have had a previous cesarean delivery are at a higher risk of uterine rupture, especially if they attempt a vaginal birth after cesarean (VBAC).
Other causes include:
- Trauma to the abdomen, such as a car accident or a fall,
- Abnormal attachment of the placenta (placenta previa),
- Prolonged or obstructed labor,
- Improper use of labor-inducing medications, or
- Improper administration of uterine stimulant drugs.
It is important to note that while a rupture can happen during pregnancy, labor, or postpartum, the majority of cases occur during labor and delivery. This is due to the increased pressure within the uterus and the physical stress placed on the uterine wall during contractions.
Signs and Symptoms of Rupture of Uterus
The signs and symptoms of a uterine rupture can vary depending on the severity of the condition. Some common signs include:
- Intense abdominal pain that does not subside with medication
- Abnormal or excessive bleeding
- A rapid drop in fetal heart rate
- A loss of uterine contractions
- A bulging or protruding mass in the abdomen
In more severe cases, the mother may experience signs of shock, including:
- Lightheadedness
- A rapid pulse
- Pale skin
- A decrease in blood pressure
It is crucial for pregnant women, especially those with risk factors or a history of uterine surgery, to be aware of these symptoms and seek immediate medical attention if they occur. Early detection and prompt intervention can significantly improve the outcome for both the mother and the baby.
- Remember to be aware of the signs and symptoms
- Seek immediate medical attention if they occur
Diagnosing Rupture of Uterus
Diagnosing a uterine rupture requires a combination of clinical evaluation, imaging studies, and monitoring of fetal well-being. Initially, the healthcare provider will assess the mother’s symptoms, perform a physical examination, and review the medical history for any predisposing factors. Additionally, continuous monitoring of the fetal heart rate is crucial to detect any signs of distress.
To confirm the diagnosis, ultrasound imaging and other radiographic studies, such as magnetic resonance imaging (MRI) or computerized tomography (CT) scan, may be used to assess the location and extent of the rupture. If fetal distress is suspected, an immediate cesarean section may be necessary to deliver the baby safely and address the rupture.
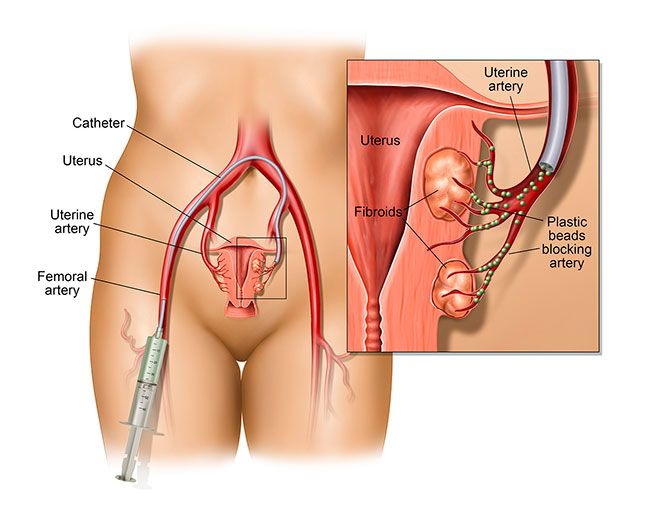
Treatment Options for Rupture of Uterus
The treatment options for a uterine rupture depend on the severity of the condition and the gestational age of the fetus.
- In cases of incomplete rupture, conservative management may be possible if the mother and the baby are stable. This may involve:
- close monitoring,
- pain management, and
-
administration of antibiotics to prevent infection.
-
However, in cases of complete rupture or when there is significant maternal or fetal distress, immediate surgical intervention is necessary. This typically involves an emergency cesarean section, where:
- the baby is delivered, and
-
the ruptured uterus is repaired.
-
In more severe cases, a hysterectomy may be required to control bleeding and prevent further complications.
––-*
Complications Associated with Rupture of Uterus
Rupture of the uterus can lead to several complications, both for the mother and the baby. For the mother, these can include severe bleeding, infection, damage to nearby organs, and the need for a hysterectomy. Maternal mortality rates associated with uterine ruptures are relatively low in developed countries, thanks to advancements in medical care and early interventions. However, in resource-limited settings, the lack of timely access to emergency obstetric care can significantly increase the risk of maternal death.
For the baby, complications may arise due to oxygen deprivation during the rupture. This can result in brain damage, cerebral palsy, or even stillbirth in severe cases. The severity of the complications depends on the length of time between the rupture and delivery, the gestational age of the fetus, and the promptness of medical intervention.
- Severe bleeding
- Infection
- Damage to nearby organs
- Need for a hysterectomy
Lack of timely access to emergency obstetric care in resource-limited settings can significantly increase the risk of maternal death.
Prevention of Rupture of Uterus
While not all cases of uterine rupture can be prevented, several measures can significantly reduce the risks. Women with a history of uterine surgeries, particularly cesarean deliveries, should discuss their options and risks with their healthcare provider when planning future pregnancies. Depending on individual circumstances, a scheduled cesarean section may be recommended to avoid the potential risks associated with vaginal delivery.
To prevent complications that could lead to a rupture, it is important to avoid unnecessary trauma to the abdomen, ensure proper prenatal care, and manage high-risk pregnancies appropriately. Additionally, close monitoring during labor and delivery, especially in cases of prolonged or obstructed labor, can help detect early signs of a potential rupture and allow for timely interventions.
Key points to consider for reducing the risks of uterine rupture:
- Women with a history of uterine surgeries, especially cesarean deliveries, should discuss options and risks with healthcare providers when planning future pregnancies.
- Scheduled cesarean section may be recommended depending on individual circumstances.
- Avoid unnecessary trauma to the abdomen.
- Ensure proper prenatal care.
- Manage high-risk pregnancies appropriately.
- Close monitoring during labor and delivery, particularly in cases of prolonged or obstructed labor, can help detect early signs of a potential rupture.
Recovery and Rehabilitation After Rupture of Uterus
The recovery and rehabilitation process following a uterine rupture can vary depending on the extent of the rupture, the type of intervention performed, and any additional complications that may have arisen.
Physical healing may take several weeks, during which the mother should rest, take prescribed medications, and closely follow any postoperative instructions provided by her healthcare provider.
Emotionally, a uterine rupture can be a traumatic experience for some women. Support from healthcare professionals, family, and friends, as well as counseling services if needed, can assist in the healing process. It is essential to allow ample time for emotional recovery and to address any feelings of guilt, grief, or anxiety that may arise.
Rupture of Uterus in Pregnancy: Unique Considerations
When a uterine rupture occurs during pregnancy, there are additional considerations that need to be taken into account. Depending on the gestational age of the fetus and the severity of the rupture, decisions regarding the management and timing of the delivery must be made. Balancing the risks of premature delivery against the potential dangers associated with a uterine rupture is crucial.
The healthcare team will carefully assess the mother and the fetus to determine the best course of action. In some cases, if the rupture is detected early and the condition is stable, conservative management with close monitoring may be possible until the fetus reaches a viable gestational age. However, if there is a high risk to the mother or the baby, immediate delivery through cesarean section may be necessary to prevent further complications.
Additional considerations include:
- Assessing the stability of the mother and fetus
- Evaluating the severity of the rupture
- Monitoring the gestational age of the fetus
- Weighing the risks of premature delivery and uterine rupture complications
“Balancing the risks and potential complications is crucial when determining the management of uterine rupture during pregnancy.”
Case Studies and Statistics on Rupture of Uterus
According to a review published in the Journal of Obstetrics and Gynaecology Canada, the incidence of uterine rupture is estimated to be around 0.05% to 0.07% of pregnancies in countries with advanced healthcare systems. However, in low-resource settings with limited access to emergency obstetric care, the incidence can be significantly higher.
Case studies highlight the importance of early detection and prompt management. One case study published in the Journal of Clinical Medicine describes a successful emergency cesarean section performed within minutes of diagnosing a complete uterine rupture. Both the mother and the baby experienced a positive outcome due to the quick intervention.
These case studies emphasize the need for increased awareness, proper antenatal care, and improved access to emergency obstetric services to prevent and manage uterine ruptures effectively.
In conclusion, rupture of the uterus is a serious complication that requires immediate medical attention. Prompt diagnosis and intervention are crucial in mitigating the risks associated with this condition. Awareness of the causes, symptoms, treatment options, and potential complications can assist healthcare professionals and women in making informed decisions to safeguard maternal and fetal health.
💡
You may need to know these questions about rupture of uterus
What happens when a uterus ruptures?
When a uterus ruptures, it poses a significant threat to both the mother and the fetus. The rupture can result in severe blood loss, placing the mother’s life in jeopardy. Meanwhile, the fetus is no longer shielded by the uterus, leading to a decrease in its heart rate and depriving it of oxygen. This lack of oxygen puts the fetus at risk of sustaining brain damage or suffocation, highlighting the critical nature of this condition that necessitates immediate medical intervention to ensure the well-being of both mother and baby.
Can a baby survive a uterine rupture?
A uterine rupture is a rare but severe complication during pregnancy that can endanger both the mother and the unborn baby. The chances of a baby surviving a uterine rupture are generally quite low, with approximately 6% not making it. The risk of serious brain injuries, like hypoxic-ischemic encephalopathy (HIE) and cerebral palsy, increases if there is any delay in responding to the rupture. Immediate medical intervention is crucial to increase the chances of a baby’s survival and minimize long-term complications. Dimitrova, D., et al. (2022).
What is the survival rate of a uterine rupture?
The survival rate of uterine rupture is approximately 89.5%. This is based on the finding that 10.5% of women with uterine rupture have unfortunately died. The median recovery time for women with uterine rupture was 8 days, while the median time for death was 3 days. The interquartile range for recovery was 7-11 days, and for death, it was 2-5 days. These statistics highlight the urgency and complexity of managing uterine rupture to improve survival rates.
What are the long term effects of uterine rupture?
Uterine rupture can have devastating long-term effects for both the baby and the mother. For the baby, it may result in lasting birth injuries such as cerebral palsy, which can affect their motor skills and overall development. Additionally, the potential consequences of uterine rupture may also lead to the unfortunate outcome of infant mortality. For the mother, she may experience long-term physical and emotional trauma, requiring extensive medical interventions and psychological support to aid in recovery and healing. Overall, the long-term effects of uterine rupture underscore the urgency for preventative measures and vigilant monitoring during pregnancy to minimize the risk and ensure the well-being of both mother and baby.
Reference source
https://www.ncbi.nlm.nih.gov/books/NBK559209/
https://my.clevelandclinic.org/health/diseases/24480-uterine-rupture
https://www.birthinjuryhelpcenter.org/uterine-rupture.html
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10054622/