Enter the realm of women’s health, where hidden struggles often remain unspoken.
Imagine a world where a condition known as senile vaginitis holds the potential to disrupt a woman’s life, causing discomfort, pain, and an array of untold challenges.
Brace yourself for a journey into the enigmatic world of vaginal atrophy and the hardships endured by those affected.
senile vaginitis
Senile vaginitis, also known as vaginal atrophy, is a condition characterized by thinning, drying, and inflammation of the vaginal walls.
It occurs due to a decrease in estrogen levels in the body, commonly seen after menopause.
This condition can cause painful intercourse and distressing urinary symptoms.
To describe vaginal atrophy and its symptoms, doctors use the term “genitourinary syndrome of menopause (GSM).”
Key Points:
- Senile vaginitis, or vaginal atrophy, is a condition involving thinning, drying, and inflammation of the vaginal walls.
- It is caused by a decrease in estrogen levels, often after menopause.
- Symptoms of senile vaginitis include painful intercourse and urinary discomfort.
- Doctors use the term “genitourinary syndrome of menopause (GSM)” to describe this condition and its symptoms.
senile vaginitis – Watch Video
💡
Pro Tips:
1. Senile vaginitis, also known as atrophic vaginitis, is a condition that primarily affects postmenopausal women and is characterized by inflammation and dryness of the vaginal walls.
2. While senile vaginitis is commonly associated with menopause, it can also occur in younger women who have undergone surgical removal of their ovaries or who have experienced premature ovarian failure.
3. Senile vaginitis can cause discomfort and pain during intercourse, leading to decreased sexual desire and pleasure.
4. Estrogen replacement therapy (ERT) or hormone replacement therapy (HRT) is often prescribed to alleviate the symptoms of senile vaginitis, as it helps restore the elasticity and lubrication of the vaginal tissues.
5. To prevent senile vaginitis, maintaining a healthy lifestyle and practicing proper vaginal hygiene can be beneficial. This includes avoiding irritants such as perfumed products, using water-based lubricants during intercourse, and regularly engaging in sexual activity to promote blood flow and maintain vaginal health.
Introduction: Senile Vaginitis And Vaginal Atrophy
Senile vaginitis, also known as vaginal atrophy, is a condition characterized by the thinning, drying, and inflammation of the vaginal walls. This condition can lead to a range of symptoms that significantly impact the quality of life for many women. Understanding the causes, symptoms, and available treatment options for senile vaginitis is essential for effective management.
Causes:
- Decreased levels of estrogen during menopause
- Certain cancer treatments like chemotherapy or radiation therapy
- Surgical removal of ovaries
Symptoms:
- Vaginal dryness
- Itching or irritation in the vaginal area
- Pain or discomfort during sexual intercourse
- Urinary problems like increased frequency or urgency
Treatment options:
- Topical estrogen therapy: Application of estrogen creams or vaginal tablets to restore vaginal health and relieve symptoms.
- Vaginal moisturizers: Regular use of water-based moisturizers to alleviate vaginal dryness.
- Lifestyle changes: Maintaining good hydration, avoiding irritants like harsh soaps or douches, and using lubricants during sexual activity.
- Systemic estrogen therapy: In certain cases, oral or transdermal estrogen therapy may be recommended.
- Regular sexual activity: Engaging in regular sexual activity may help increase blood flow to the vaginal area and promote natural lubrication.
“Effective management of senile vaginitis requires understanding its causes, recognizing the symptoms, and exploring the available treatment options.”
- Increase in estrogen levels during menopause
- Cancer treatments such as chemotherapy or radiation
-
Surgical removal of the ovaries
-
Vaginal dryness
- Itching or irritation in the vaginal area
- Pain or discomfort during sexual intercourse
-
Urinary problems like increased frequency or urgency
-
Topical estrogen therapy: Estrogen creams or vaginal tablets applied to restore vaginal health and relieve symptoms.
- Vaginal moisturizers: Regular use of water-based moisturizers to alleviate vaginal dryness.
- Lifestyle changes: Maintaining good hydration, avoiding irritants like harsh soaps or douches, and using lubricants during sexual activity.
- Systemic estrogen therapy: In some cases, oral or transdermal estrogen therapy may be recommended.
- Regular sexual activity: Engaging in regular sexual activity may help increase blood flow to the vaginal area and promote natural lubrication.
Decrease In Estrogen Levels: Leading Cause Of Vaginal Atrophy
The primary cause of vaginal atrophy is a decrease in estrogen levels in the body. Estrogen plays a crucial role in maintaining the health and function of vaginal tissues. As women age, especially during and after menopause, estrogen levels naturally decline, leading to thinning and inflammation of the vaginal walls. This hormonal imbalance deprives the vaginal tissues of moisture and elasticity, causing discomfort and irritation.
Vaginal Atrophy: Commonly Experienced After Menopause
Vaginal atrophy primarily occurs after menopause, around the age of 50, when estrogen production from the ovaries stops. The decrease in estrogen levels during this period escalates the risk of developing vaginal atrophy. Nevertheless, it is crucial to acknowledge that hormonal imbalances or medical treatments can also trigger vaginal atrophy in women who have not yet gone through menopause.
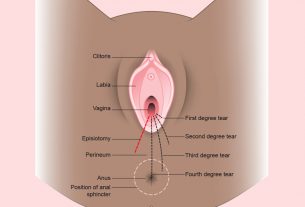
Painful Intercourse: A Main Symptom Of Vaginal Atrophy
One of the main symptoms of vaginal atrophy is painful intercourse, also known as dyspareunia. The thinning and drying of the vaginal walls can lead to a lack of lubrication and increased friction during sexual activity. This can cause significant discomfort and pain for women, leading to a decreased interest in sexual intercourse and strain on relationships.
It is vital for women experiencing painful intercourse to seek medical intervention to address the underlying cause and find suitable treatment options.
- Vaginal atrophy can cause painful intercourse (dyspareunia).
- Thinning and drying of the vaginal walls can result in lack of lubrication and increased friction during sexual activity.
- Painful intercourse can lead to decreased interest in sexual intercourse and strain on relationships.
“It is vital for women experiencing painful intercourse to seek medical intervention to address the underlying cause and find suitable treatment options.”
Distressing Urinary Symptoms: Associated With Vaginal Atrophy
Vaginal atrophy not only leads to painful intercourse but can also result in distressing urinary symptoms. As the condition progresses, women may face several issues such as frequent urinary tract infections (UTIs), urinary urgency, urinary incontinence, and a higher risk of urinary tract complications. These symptoms can greatly impact daily activities and overall quality of life. It is of utmost importance to consult with a healthcare professional for accurate diagnosis and effective management of these urinary symptoms.
Genitourinary Syndrome Of Menopause (GSM): Definition And Description
Doctors use the term “genitourinary syndrome of menopause (GSM)” to describe vaginal atrophy and its associated symptoms. GSM encompasses the changes that occur in the urogenital tract due to decreased estrogen. This syndrome includes symptoms such as vaginal dryness, irritation, itching, burning, urinary symptoms, and even sexual dissatisfaction. Understanding GSM allows healthcare providers to provide a comprehensive approach to managing vaginal atrophy and its impact on a woman’s overall well-being.
Impact Of Vaginal Atrophy On Quality Of Life
Vaginal atrophy can significantly affect a woman’s quality of life, both physically and emotionally. Symptoms, including painful intercourse and urinary issues, can cause distress and frustration. Unfortunately, many women feel embarrassed or hesitant to seek help, which only worsens the effects of this condition. Hence, it is essential to recognize the potential impact of vaginal atrophy in order to encourage women to seek appropriate medical attention and support.
Managing Vaginal Atrophy: Treatment Options Available
Thankfully, there are various treatment options available to manage vaginal atrophy and alleviate its associated symptoms. Hormone replacement therapy (HRT) is a common treatment method that involves the administration of estrogen to restore hormonal balance. This can be prescribed in the form of creams, tablets, or vaginal rings. Non-hormonal options, such as vaginal moisturizers and lubricants, can also provide relief by increasing vaginal lubrication. Additionally, lifestyle changes and certain exercises may help improve the overall strength and flexibility of vaginal tissues.
Preventive Measures: Minimizing The Risk Of Vaginal Atrophy
While vaginal atrophy is commonly associated with menopause, there are preventive measures that women can take to minimize the risk of developing this condition.
- Leading a healthy lifestyle that includes a balanced diet, regular exercise, and avoidance of tobacco and excessive alcohol consumption can contribute to overall vaginal health.
- Moreover, practicing safe sex, maintaining regular sexual activity, and using water-based lubricants during intercourse can also help prevent the onset of vaginal atrophy.
Conclusion: Understanding And Addressing Vaginal Atrophy And GSM
Senile vaginitis, also known as vaginal atrophy, primarily affects women after menopause due to declining estrogen levels. This condition can lead to various troubling symptoms such as painful intercourse and urinary issues, significantly impacting a woman’s quality of life. Understanding and recognizing vaginal atrophy and its related symptoms, collectively known as genitourinary syndrome of menopause (GSM), is essential for individuals to seek proper medical attention and explore available treatment options. By effectively managing this condition, women can regain control over their sexual health and overall well-being.
💡
You may need to know these questions about senile vaginitis
What are the symptoms of senile vulvovaginitis?
Senile vulvovaginitis is characterized by various symptoms that women may experience as they age. These include vulvovaginal dryness, causing discomfort and an itchy sensation. Alongside this, women may also encounter dyspareunia, which is pain during sexual intercourse, and post-coital pain in the labia minora or deeper within the vaginal vault. Additionally, abnormal vaginal discharge, recurrent urinary tract infections, urethral pain, hematuria, and urinary incontinence can be present. These symptoms collectively contribute to the experience of senile vulvovaginitis, impacting the well-being and quality of life of affected individuals.
1) What are the common symptoms of senile vaginitis and how does it differ from other forms of vaginal infections?
Senile vaginitis, also known as atrophic vaginitis or vaginal atrophy, is a condition that commonly affects postmenopausal women. It is characterized by various symptoms including vaginal dryness, itching, burning sensation, discharge, and discomfort during sexual intercourse. The decreased estrogen levels in the body during menopause cause thinning and drying of the vaginal walls, leading to these symptoms.
Unlike other forms of vaginal infections, such as bacterial vaginosis or yeast infections, senile vaginitis is not caused by an infection or an overgrowth of bacteria or yeast. It is primarily due to hormonal changes that occur with aging. This differentiates it from other forms of vaginal infections and requires a different approach to treatment. While other infections may require antimicrobial medications, senile vaginitis is usually treated with vaginal moisturizers or lubricants, hormone replacement therapy, or certain topical creams or medications that help to alleviate symptoms and restore vaginal health.
2) What are the potential causes or risk factors for developing senile vaginitis in older women?
Senile vaginitis, also known as atrophic vaginitis or vaginal atrophy, refers to the inflammation and thinning of the vaginal walls in older women, primarily occurring as a result of decreased estrogen levels during menopause. Estrogen plays a crucial role in maintaining the health and thickness of the vaginal lining. When estrogen declines, the vagina loses elasticity, becomes drier, and more susceptible to irritation and infection. Other potential causes or risk factors for developing senile vaginitis include certain medical conditions, such as diabetes or immune system disorders, as well as smoking, poor nutrition, and certain medications that can affect estrogen levels.
In addition to natural hormonal changes, external factors and medical conditions can contribute to the development of senile vaginitis in older women. These may include chronic diseases like diabetes, which can lead to higher glucose levels in vaginal tissues, increasing the risk of infections. Similarly, immune system disorders or conditions that compromise the immune system can make women more susceptible to infections that can result in senile vaginitis. Certain medications, including hormone therapy, anti-estrogen drugs, and some antidepressants, can also affect estrogen levels and contribute to vaginal thinning and inflammation. Finally, lifestyle factors such as smoking and poor nutrition can also increase the risk of developing senile vaginitis.
3) Are there any specific treatment options or management strategies available for senile vaginitis, and how effective are they in providing relief for the associated symptoms?
There are specific treatment options and management strategies available for senile vaginitis. The primary focus is on relieving the associated symptoms, such as dryness, itching, and pain during intercourse. Hormone replacement therapy (HRT), either through topical or systemic administration, is a common treatment approach. It helps to replenish estrogen levels in the vaginal tissues, restoring moisture and elasticity. Non-hormonal options like vaginal moisturizers and lubricants can also be helpful in relieving symptoms. These treatments are generally effective in providing relief for senile vaginitis symptoms, but the success may vary depending on individual responses and overall health conditions.
Apart from medical interventions, self-care measures can also play a role in managing senile vaginitis symptoms. Simple strategies like regular vaginal hygiene, avoiding irritants, and wearing loose, breathable clothing can contribute to symptom relief. It is always recommended to consult a healthcare professional for an accurate diagnosis and to discuss appropriate treatment options for senile vaginitis.
Reference source
https://www.mayoclinic.org/diseases-conditions/vaginal-atrophy/symptoms-causes/syc-20352288
https://www.ncbi.nlm.nih.gov/books/NBK564341/
https://my.clevelandclinic.org/health/diseases/15500-vaginal-atrophy
https://www.aafp.org/pubs/afp/issues/2000/0515/p3090.html