Septic shock: a mere mention of these two words sends a shiver down our spines.
It is a haunting reality, a menacing condition that can grip even the healthiest among us.
Picture this: a ferocious battle between our body and a deadly infection.
The stakes couldn’t be higher.
Will our heroic immune system prevail, or will we succumb to the dark clutches of septic shock?
Join us on this journey as we navigate the treacherous terrain of this life-threatening condition, uncovering the secrets to survival and the measures taken to combat this silent assassin.
Brace yourself, for the fight for survival begins now.
septic shock
Septic shock is a life-threatening condition that occurs when blood pressure drops to a dangerously low level after an infection.
It can be caused by any type of bacteria, fungi, or viruses.
People with weakened immune systems are more at risk.
Treatment involves admission to an intensive care unit (ICU) for organ support and infection treatment.
This may include oxygen therapy, intravenous fluids, medication to increase blood flow, antibiotics, and, in severe cases, surgery.
Oxygen therapy can be administered through a mask, tube, or ventilator, while intravenous fluids help raise blood pressure.
Inotropic medicines stimulate the heart to increase blood flow, and vasopressors narrow blood vessels to improve organ function.
Antibiotics are used to treat associated bacterial infections, and surgery may be necessary in severe cases.
Key Points:
- Septic shock is a life-threatening condition caused by an infection that leads to a dangerous drop in blood pressure.
- Any type of bacteria, fungi, or viruses can cause septic shock.
- Individuals with weakened immune systems are more vulnerable to septic shock.
- Treatment requires ICU admission for organ support and infection treatment.
- Treatment options may include:
- Oxygen therapy
- Intravenous fluids
- Medication to increase blood flow
- Antibiotics
- Surgery in severe cases
- Oxygen therapy can be administered through a mask, tube, or ventilator, while intravenous fluids help raise blood pressure.
septic shock – Watch Video
💡
Pro Tips:
1. Septic shock is a life-threatening condition caused by an overwhelming bacterial infection that rapidly spreads throughout the entire body, leading to multiple organ failure.
2. Septic shock is often characterized by a significant decrease in blood pressure, which can result in the body’s vital organs being deprived of oxygen and nutrients.
3. While septic shock most commonly occurs as a result of bacterial infections, it can also be triggered by certain viral, fungal, or parasitic infections.
4. Although septic shock primarily affects older adults and individuals with weakened immune systems, it can also occur in younger, otherwise healthy individuals.
5. Septic shock is often treated in intensive care units (ICUs) using a combination of antibiotics, fluid resuscitation, vasopressors, and other supportive therapies.
Definition And Causes Of Septic Shock
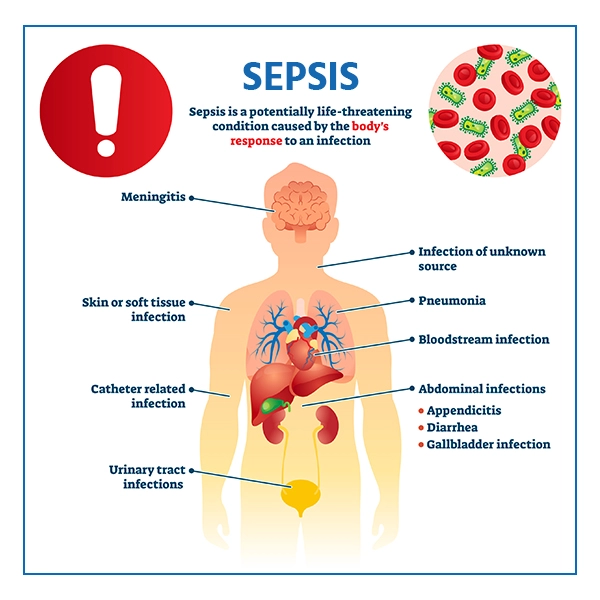
Septic shock is a life-threatening condition that occurs when blood pressure drops to a dangerously low level after an infection. The infection can be caused by bacteria, fungi, or viruses.
When an infection occurs, the body’s immune system initiates an inflammatory response to fight off the pathogens. However, in some cases, this response can become overwhelming and lead to a cascade of events that impair organ function and cause a drop in blood pressure.
The immune response triggers the release of various substances, such as cytokines and other inflammatory mediators, which can result in widespread inflammation and damage throughout the body. This process, known as sepsis, can progress rapidly and lead to septic shock if not promptly treated.
Septic shock is characterized by a significant decrease in blood pressure, which can impair the delivery of oxygen and nutrients to vital organs, such as the heart, lungs, and brain. If left untreated, septic shock can be fatal.
Risk Factors For Septic Shock
Certain individuals are more at risk of developing septic shock. These include:
- People with weakened immune systems, such as those with HIV/AIDS, undergoing chemotherapy, or taking immune-suppressing medications.
- Individuals with chronic illnesses, such as diabetes, liver disease, or kidney disease, that may compromise their immune systems and make them more susceptible to infections and septic shock.
Additional risk factors for septic shock include:
- Age, with both very young and elderly individuals being more prone to the condition.
- Recent surgical procedures.
- Invasive medical devices, such as urinary catheters or ventilators.
- A history of recurrent infections.
It is crucial for individuals with these risk factors to be vigilant about preventing infections and to seek prompt medical attention if they suspect an infection.
Treatment And Care In The Intensive Care Unit
When a patient is diagnosed with septic shock, immediate treatment and care in an intensive care unit (ICU) are essential. The goal of treatment is to stabilize the patient’s condition, restore blood pressure and blood flow to vital organs, and eradicate the underlying infection. The ICU provides specialized equipment, monitoring, and a multidisciplinary team of healthcare professionals who can deliver prompt and intensive care.
Treatment for septic shock typically involves a combination of interventions. Oxygen therapy is often administered through a mask, tube, or ventilator to ensure adequate oxygenation of the body. Intravenous fluids are given to expand blood volume and increase blood pressure. Inotropic medicines may be used to stimulate the heart and improve blood flow to organs. Furthermore, vasopressors are utilized to narrow blood vessels, increase blood pressure, and optimize organ function.
In addition to these interventions, antibiotics are prescribed to treat associated bacterial infections. The choice of antibiotics depends on the specific infection and its location. It is crucial to administer the appropriate antibiotics promptly, ideally within the first hour of recognition, to improve outcomes. In severe cases of septic shock where blood pressure and blood flow remain dangerously low despite other treatments, surgical intervention may be necessary to address the underlying cause and restore proper circulation.
Oxygen Therapy For Septic Shock Patients
One of the primary treatment modalities for septic shock is oxygen therapy. This intervention ensures that the body receives adequate oxygenation, as low blood pressure and compromised blood flow can lead to decreased oxygen delivery to essential organs.
Oxygen therapy is administered through various methods, depending on the patient’s condition and the severity of respiratory distress.
- For patients with mild respiratory compromise, oxygen can be delivered through a face mask. This allows them to inhale a higher concentration of oxygen, increasing the oxygen saturation in their blood.
- However, when respiratory distress is more severe, a tube may be inserted through the nose or mouth and down into the trachea, and the patient can be connected to a mechanical ventilator that delivers oxygen directly to the lungs.
The goal of oxygen therapy is to maintain oxygen saturation within a safe range while supporting the body’s oxygen demands. The healthcare team closely monitors the patient’s oxygen levels and adjusts the oxygen delivery accordingly.
Oxygen therapy, in conjunction with other treatments, plays a critical role in stabilizing septic shock patients and optimizing their chances for recovery.
Intravenous Fluids To Increase Blood Pressure
Intravenous (IV) fluids play a crucial role in the treatment of septic shock. These fluids are directly administered into the bloodstream using a catheter, bypassing the gastrointestinal system. By rapidly increasing the body’s fluid volume, IV fluids aim to elevate blood pressure. This is essential to ensure sufficient blood flow to vital organs and prevent organ dysfunction.
Septic shock causes a decrease in blood pressure due to the dilation of blood vessels and loss of vascular tone. IV fluids, commonly in the form of saline solutions, restore blood pressure by compensating for the reduced volume and improving cardiac output. However, it is important to carefully monitor the administration of IV fluids to prevent fluid overload and other adverse effects. The healthcare team continually evaluates the patient’s response to the fluids and adjusts the rate and volume as necessary.
Early initiation of intravenous fluid resuscitation is often necessary in the treatment of septic shock to address hypoperfusion and support the function of vital organs. However, it is crucial to maintain a delicate balance, as excessive fluid administration can lead to complications such as pulmonary edema, impaired tissue perfusion, and electrolyte imbalances.
Inotropic Medicines To Improve Blood Flow
In septic shock, the heart’s ability to pump blood effectively is compromised, contributing to decreased blood flow to vital organs. To improve blood flow and optimize organ perfusion, inotropic medicines may be administered. These medications help stimulate the heart muscle, increasing the strength and efficiency of its contractions.
Inotropes work by acting directly on the heart’s cells, enhancing the release and utilization of calcium, which plays a crucial role in cardiac muscle contraction. By improving contractility, the heart can pump more blood with each beat, leading to increased blood flow throughout the body.
Inotropic agents commonly used in septic shock include:
- Dobutamine
- Dopamine
- Epinephrine
The choice of inotropic medication depends on the patient’s condition, hemodynamic stability, and the healthcare team’s assessment. As with any medication, inotropic medicines have potential side effects, and their administration requires close monitoring. The dosage and duration of use are determined on an individual basis, tailored to the patient’s response and ongoing cardiovascular support needs.
Vasopressors To Increase Blood Pressure
In septic shock, the drop in blood pressure can severely impair proper organ function and compromise tissue perfusion. Vasopressors are a crucial part of septic shock treatment, as they help increase blood pressure by constricting blood vessels and improving systemic vascular resistance.
Commonly used vasopressor medications in septic shock include norepinephrine and vasopressin. These drugs act on alpha-adrenergic receptors located on blood vessels, causing vasoconstriction and leading to increased blood pressure. By narrowing the blood vessels, vasopressors redirect blood flow to vital organs, improving their oxygenation and function.
Vasopressors are administered intravenously and are titrated carefully according to the patient’s response, blood pressure, and organ perfusion. Correct dosing and close monitoring are crucial, as excessive use of vasopressors can lead to adverse effects such as tissue ischemia, impaired renal function, or arrhythmias. The healthcare team continuously assesses the patient’s hemodynamic status to ensure optimal vasopressor therapy and make any necessary adjustments.
Antibiotics For Treating Infections
In septic shock, infections are often the underlying cause that triggers the body’s inflammatory response and subsequent decrease in blood pressure. Prompt administration of appropriate antibiotics is crucial in managing septic shock effectively and improving patient outcomes. Antibiotics target and kill the pathogens responsible for the infection, halting the progression of sepsis and reducing the risk of complications.
The choice of antibiotics depends on the suspected or identified source of infection and the likely pathogens involved. Broad-spectrum antibiotics are commonly used initially to cover a wide range of bacteria, fungi, and viruses. As the infection becomes more precisely identified, the healthcare team may adjust the antibiotic regimen to target the specific pathogens involved.
Timing is crucial when initiating antibiotics in septic shock. The goal is to administer the appropriate antibiotics promptly, ideally within the first hour of recognition. Delayed administration can lead to worsened outcomes, including increased mortality rates. Therefore, healthcare providers should be vigilant in promptly identifying signs of septic shock and initiating the appropriate antibiotic therapy as soon as possible.
- Prompt administration of appropriate antibiotics
- Target and kill the pathogens responsible for the infection
- Use broad-spectrum antibiotics initially
- Adjust antibiotic regimen according to identified pathogens
- Timing is crucial – administer antibiotics within the first hour of recognition
Surgical Intervention For Severe Septic Shock Cases
In severe cases of septic shock where blood pressure and blood flow remain dangerously low despite other treatments, surgical intervention may be necessary. Surgical procedures are reserved for patients who do not respond adequately to medical management or those with an identified source of infection that requires direct intervention.
There are various surgical interventions that may be performed in septic shock, depending on the underlying cause. For example, if the infection originates from a localized area, such as the abdomen, the surgeon may need to drain abscesses or remove infected tissues. In cases of severe lung infection, a surgical procedure called a lung decortication may be necessary to remove infected and damaged lung tissue.
Surgical intervention aims to address the underlying cause of septic shock, improve blood flow, and restore organ function. The decision to proceed with surgery is carefully considered by the healthcare team, weighing the potential risks and benefits. Timing is critical, and prompt intervention can be life-saving for patients with severe septic shock.
Conclusion: Addressing Blood Pressure And Blood Flow In Septic Shock
Septic shock is a life-threatening condition characterized by a significant drop in blood pressure following an infection. It can be caused by bacteria, fungi, or viruses and can rapidly progress if not promptly treated. Individuals with weakened immune systems and certain risk factors are particularly vulnerable to septic shock.
Treatment and care for septic shock primarily occur in intensive care units (ICUs), where patients receive specialized care aimed at stabilizing their condition and eradicating the underlying infection. Various interventions are utilized to address blood pressure and blood flow, including oxygen therapy, intravenous fluids, inotropic medications, and vasopressors.
Additionally, antibiotics play a crucial role in treating the underlying infection and preventing further complications. Prompt administration of appropriate antibiotics is essential in improving patient outcomes. In severe cases where blood pressure and blood flow remain dangerously low, surgical intervention may be necessary to address the underlying cause and restore proper circulation.
Awareness of septic shock and its risk factors, coupled with early recognition and immediate medical attention, are paramount for preventing and effectively managing this life-threatening condition. With early intervention and comprehensive multidisciplinary care, the prognosis for septic shock patients can be improved, increasing their chances of recovery and survival.
💡
You may need to know these questions about septic shock
What are the warning signs of septic shock?
Warning signs of septic shock include feeling lightheaded or faint, experiencing confusion or disorientation, slurred speech, severe muscle pain, severe breathlessness, not urinating for a day, and having cold, clammy, pale, or mottled skin with a grey appearance. These symptoms may indicate a potentially life-threatening condition where the body’s response to an infection leads to widespread inflammation and organ dysfunction. Prompt medical attention should be sought if these signs are present to diagnose and treat septic shock.
What are the 3 stages of septic shock?
The three stages of septic shock are sepsis, severe sepsis, and septic shock. Sepsis is characterized by a life-threatening response of the immune system to an infection. In this stage, the body shows signs of inflammation, such as fever, increased heart rate, and rapid breathing. If sepsis progresses, it can lead to severe sepsis, where organs start to malfunction or fail. Finally, in septic shock, there is a significant drop in blood pressure, making it challenging for organs to receive the necessary oxygen and nutrients. This stage can be life-threatening and requires immediate medical attention.
Can a person survive septic shock?
Surviving septic shock is possible, although it can be a life-threatening condition. Septic shock occurs when an infection in the body triggers a severe inflammatory response, leading to organ failure. While organ failure can be fatal in some cases, many individuals who receive prompt medical intervention and aggressive treatment have a chance of survival. With timely medical care, intensive support, and a comprehensive treatment plan, individuals who make it through septic shock can often recover and resume their normal lives. However, it is crucial to acknowledge the seriousness of the condition and seek immediate medical attention to maximize the chances of survival and a successful recovery.
What are the odds of surviving septic shock?
The odds of surviving septic shock can be challenging, with global statistics suggesting a grim outcome for one-third of individuals afflicted with sepsis. Survivors, though fortunate, are often burdened with lasting repercussions. These can consist of various life-altering consequences including post-traumatic stress disorder, chronic pain and fatigue, organ dysfunction, and possibly even amputations. While the road to recovery may be formidable, advancements in medical interventions and increased awareness of sepsis provide hope for improving the odds in the future.
Reference source
https://www.nhsinform.scot/illnesses-and-conditions/blood-and-lymph/septic-shock
https://www.nidirect.gov.uk/news/recognising-signs-and-symptoms-sepsis
https://my.clevelandclinic.org/health/diseases/23255-septic-shock
https://newsinhealth.nih.gov/2014/08/surviving-sepsis