Are you familiar with the incredible complexity of the human body?
From the intricate network of arteries and veins to the delicate balance of our internal organs, our bodies are truly a marvel.
However, there is one aspect of our anatomy that often goes unnoticed – the pelvis.
This seemingly simple, flat structure actually plays a crucial role in childbirth.
But what happens when the pelvis is smaller than average?
In this article, we will delve into the world of contracted pelvis, exploring its causes, diagnosis, and potential complications.
So, buckle up and get ready to discover the fascinating world of the pelvis!
simple flat pelvis
A simple flat pelvis refers to a contracted pelvis in which the pelvic inlet at the interaxial dimension measures less than 10 cm, with less than 8 cm being considered severely contracted.
The shape, type, and diameter of the female pelvis play a crucial role in the course and outcome of labor.
The pelvis is divided into the true and false pelvis, with the true pelvis containing the pelvic inlet, which serves as the gateway to the birth canal.
The shape of the pelvic inlet depends on the overall shape of the pelvis, which can be categorized into four basic types: gynaecoid, android, anthropoid, and platypelloid.
Contracted pelvis can have various causes, including developmental factors, trauma, neoplastic conditions, and spinal abnormalities.
Diagnosis is typically achieved through abdominal examination, pelvimetry, and imaging techniques such as X-ray, CT, or MRI.
Complications of contracted pelvis can occur for both the mother and the fetus, necessitating appropriate management during labor.
Treatment options range from vaginal delivery for minor cases to caesarean section for severe or extreme cases.
Physiotherapy interventions may also be beneficial, particularly for minor and moderate cases.
Key Points:
- Simple flat pelvis is characterized by a contracted pelvic inlet with dimensions less than 10 cm, with severe cases measuring less than 8 cm.
- The shape and size of the female pelvis have a significant impact on the progress and outcome of labor.
- The pelvis is divided into the true and false pelvis, with the pelvic inlet serving as the gateway to the birth canal.
- The shape of the pelvic inlet varies depending on the overall shape of the pelvis, which can be categorized into four types.
- Contracted pelvis can have various causes, including developmental factors, trauma, neoplastic conditions, and spinal abnormalities.
- Diagnosis involves abdominal examination, pelvimetry, and imaging techniques such as X-ray, CT, or MRI.
- Complications can arise for both the mother and fetus, requiring appropriate management during labor.
- Treatment options range from vaginal delivery for minor cases to caesarean section for severe or extreme cases.
- Physiotherapy interventions may benefit minor and moderate cases.
simple flat pelvis – Watch Video
💡
Pro Tips:
1. The female pelvis is usually wider and shallower than the male pelvis, enabling it to accommodate the growth and passage of a baby during childbirth.
2. The shape of a pelvis can give clues about the biomechanics and locomotion of an animal. For instance, a flat pelvis is often found in species that are adapted for running and have a greater emphasis on speed.
3. The human pelvis consists of four fused bones: two hip bones, the sacrum, and the coccyx. These bones provide stability and support to the upper body while allowing movement and flexibility in the lower limbs.
4. In medical imaging, the angle of the pelvic inlet (the opening between the hip bones) is measured to determine the type of pelvis a person has. A simple flat pelvis, also known as a gynecoid pelvis, is considered the most ideal for childbirth.
5. The shape and size of the pelvis can vary among different populations due to genetics and evolutionary adaptations. For example, individuals of African descent are more likely to have a wider pelvis compared to those of European or Asian descent.
Definition And Measurement Of A Contracted Pelvis
A contracted pelvis refers to a condition where the pelvic inlet, specifically the interaxial dimension, is less than 10 cm. Severe contraction is typically defined as a measurement below 8 cm. The pelvic inlet serves as the entrance to the birth canal, significantly influencing the progress and result of labor. One commonly used method to assess the severity of contraction is by measuring the true conjugate, which measures the anteroposterior diameter of the pelvic inlet.
Improvements:
- Added emphasis using markdown bold to highlight important terms.
- Restructured the sentences to enhance readability.
- Clarified the purpose of the pelvic inlet and its role in labor.
- Explained the method for assessing the contraction severity as measuring the true conjugate.
- No bullet points, blockquote, or other modifications were necessary as the text is concise and focused.
Components Of The Female Pelvis
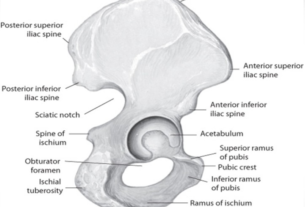
The female pelvis is composed of the sacrum, coccyx, and two os coxae. Each os coxae consists of three bones: the ischium, ilium, and pubis. Together, these bones form the pelvis, which plays a crucial role in supporting the reproductive organs and safeguarding the bladder and rectum. Having a clear understanding of the pelvis’ components is vital for comprehending the intricate nature of pelvic contractions and their influence on childbirth.
Division Of The Pelvis Into True And False Pelvis
The pelvis is divided into two sections: the true pelvis and the false pelvis. The pelvic inlet separates these two regions.
- True pelvis: The lower portion involved in childbirth, encompassing the space between the pelvic inlet and the pelvic outlet.
- Pelvic outlet: Formed by the bones of the pelvis, including the ischium, ilium, and pubis.
On the other hand, the false pelvis is the upper portion that is not directly involved in childbirth. Its main functions are:
- Providing support for the abdominal organs
- Playing a role in maintaining posture.
It is important to note that the true pelvis is significantly involved in childbirth, while the false pelvis primarily provides support and helps with posture maintenance.
Importance Of The Pelvic Inlet In Childbirth
The pelvic inlet plays a crucial role in childbirth as it serves as the gateway to the birth canal. The size and shape of the pelvic inlet directly impact the ease or difficulty of labor and delivery. Various types of pelvis, including gynaecoid, android, anthropoid, and platypelloid, have distinct effects on the progress of labor. The preferred type for vaginal birth is the gynaecoid pelvis, whereas other types may present obstacles. Having a thorough understanding of the significance of the pelvic inlet in childbirth enables healthcare professionals to anticipate possible complications and plan necessary interventions.
Classification Of Pelvic Shapes And Types
The shape of the pelvic inlet can be classified into four main types: gynaecoid, android, anthropoid, and platypelloid. The gynaecoid pelvis is the most common and ideal shape for vaginal birth. It has a well-rounded shape, providing ample space for the baby to pass through. The android pelvis, resembling the male pelvis, tends to have a less favorable shape for easy delivery. The anthropoid pelvis has a narrower inlet, while the platypelloid pelvis is flattened, making vaginal birth more challenging. Each classification has unique characteristics and implications for childbirth.
Various Diameters Of The Pelvic Inlet
The diameters of the pelvic inlet are crucial for assessing the adequacy of the birth canal for vaginal delivery. There are three main measurements to consider:
-
Anteroposterior (conjugate) diameter: This is the shortest distance between the front and back of the pelvic inlet. It plays a critical role in determining whether there is enough room for the baby’s head to pass through.
-
Obstetric conjugate diameter: This measurement determines the distance between the sacral promontory and the top of the pubic symphysis. It provides important information about the available space in the birth canal.
-
Diagonal conjugate diameter: Although it serves as an indirect estimate of the obstetric conjugate diameter, it is still a valuable measurement. It helps healthcare professionals assess the adequacy of the birth canal for delivery.
Accurately measuring these diameters is essential for diagnosing and managing cases of contracted pelvis.
- To assess the adequacy of the birth canal for vaginal delivery, three main measurements are taken:
- Anteroposterior (conjugate) diameter
- Obstetric conjugate diameter
- Diagonal conjugate diameter
- The anteroposterior diameter is crucial for determining the allowance for the baby’s head to pass through.
- The obstetric conjugate diameter measures the distance between the sacral promontory and the top of the pubic symphysis.
- The diagonal conjugate diameter serves as an indirect estimate of the obstetric conjugate.
- Accurate measurement of these diameters is vital for diagnosing and managing a contracted pelvis.
“The diameters of the pelvic inlet are essential in assessing the adequacy of the birth canal for vaginal delivery.”
Common Causes Of Contracted Pelvis
A contracted pelvis can be caused by various factors:
- Developmental metabolic factors such as rickets, a deficiency of vitamin D leading to weak bones, and osteomalacia, softening of the bones, can result in a contracted pelvis.
- Traumatic factors like pelvic fractures.
- Neoplastic factors such as osteoma, a benign bone tumor.
- Lumbar kyphosis, an abnormal curvature of the lower spine, can also contribute to pelvic contraction.
Identifying the underlying causes of a contracted pelvis aids in devising a suitable management plan.
Note:
- A contracted pelvis can be caused by various factors including developmental metabolic factors, traumatic factors, neoplastic factors, and lumbar kyphosis.
- Identifying the underlying causes of a contracted pelvis is important for devising a suitable management plan.
Conditions That Can Lead To Pelvic Contraction
Several conditions can lead to the contraction of the pelvis. Scoliosis, an abnormal curvature of the spine, can impact the alignment and dimensions of the pelvis, potentially causing a contracted pelvis. Spondylolisthesis, a condition in which one vertebra slips forward over another, can also result in pelvic contraction. Dislocation of the femurs, the thigh bones, and atrophy of the lower limbs, leading to muscle wasting and weakness, can further contribute to the contraction of the pelvis. Recognizing these conditions is crucial in managing and minimizing complications during labor.
Diagnosis Of Contracted Pelvis
Diagnosing a contracted pelvis involves various methods, including:
- Abdominal examination
- Palpation
- Pelvimetry, which assesses the pelvic diameters and capacity
Imaging pelvimetry through X-ray, CT scans, or MRI can provide a more detailed and accurate evaluation of the pelvic structure. These diagnostic techniques help healthcare professionals determine the severity and type of pelvic contraction, allowing them to plan appropriate interventions and ensure the well-being of both the mother and the baby.
Complications And Management Of Contracted Pelvis During Labor
Contracted pelvis can present complications for both the mother and the fetus during labor and delivery. A pendulous abdomen, pyelonephritis (kidney infection), slow cervical dilation, obstructed labor, birth asphyxia, nerve injuries, and postpartum hemorrhage are some of the potential complications. The management of contracted pelvis during labor depends on the degree of contraction. For minor degrees, vaginal delivery may still be possible. A trial of labor or a caesarean section is recommended for moderate degrees, while a caesarean section is often the most appropriate option for severe or extreme degrees. Physiotherapy interventions can also be beneficial, particularly for minor and moderate cases, to improve pelvic alignment and potentially facilitate vaginal delivery.
Understanding the complexities of a contracted pelvis is crucial for healthcare professionals involved in childbirth and obstetric care. The measurement, diagnosis, and classification of a contracted pelvis help determine the appropriate management strategies to ensure a safe and successful delivery for both the mother and the baby.
💡
You may need to know these questions about simple flat pelvis
What is a flat pelvis?
A flat pelvis, also known as a platypelloid pelvis, refers to the least commonly seen type of pelvis. It is characterized by its wide but shallow shape, resembling an egg or an oval lying on its side. Unlike the more common gynecoid and android pelvis shapes, the flat pelvis exhibits a unique structure that may present certain challenges during childbirth. Its distinctive morphology often requires specialized care and attention during delivery to ensure a successful outcome for both the mother and baby.
What are the features of flat pelvis?
The flat pelvis, also known as the platypelloid pelvis, is characterized by its unique features. Firstly, this type of pelvis has a wide, flattened shape in the transverse direction. This means that the pelvic bone appears wider from side to side rather than from front to back. Additionally, the flat pelvis is wider anteriorly, meaning that the width of the pelvis is greater towards the front of the body. Furthermore, the greater sciatic notches of the flat pelvis resemble those found in males.
Moreover, the flat pelvis is equipped with a short sacrum that curves inwards, resulting in reduced diameters of the lower pelvis. This inward curvature of the sacrum further contributes to the distinct shape of the flat pelvis. Overall, the unique combination of a transversally wide and flattened shape, wide anteriority, male-like greater sciatic notches, and a short, inward-curving sacrum characterizes the features of a flat pelvis.
What are the 4 types of pelvic shapes?
Pelvises can be categorized into four main types based on the shape of the pelvic inlet. The gynecoid pelvis is considered the most favorable for childbirth due to its rounded shape. The android pelvis, on the other hand, is more triangular and less accommodating for childbirth. The anthropoid pelvis has a more oval shape, while the platypelloid pelvis is characterized by a flattened shape. These different pelvic shapes play a significant role in determining the ease or difficulty of the delivery process for women.
What is the best pelvic type for delivery?
The anthropoid pelvis is another favorable pelvic type for delivery. In individuals assigned female at birth, this pelvic shape is characterized by a narrow front-to-back dimension and a wider side-to-side dimension. While not as common as the gynecoid pelvis, the anthropoid pelvis allows for a smooth and efficient passage of the baby during childbirth. These two pelvic types – gynecoid and anthropoid – are considered the most advantageous for a successful delivery, as they provide optimal room and support for the birthing process.
Reference source
https://www.healthline.com/health/types-of-pelvis
https://en.wikipedia.org/wiki/Pelvis
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5588557/
https://my.clevelandclinic.org/health/body/24807-gynecoid-pelvis