Imagine a world where the simple act of getting your period feels like a battle.
Imagine excruciating pain that leaves you curled up in bed, longing for relief.
Welcome to the world of spasmodic dysmenorrhea, a condition that plunges countless women into a monthly struggle.
Join us as we explore the causes, treatment options, and tales of triumph over this relentless adversary.
spasmodic dysmenorrhea
Spasmodic dysmenorrhea is a condition that causes severe and painful menstrual cramps during menstruation.
It is characterized by muscle spasms in the uterus, leading to significant discomfort and sometimes interfering with daily activities.
Treatment options for this condition may include over-the-counter pain relievers, hormonal birth control methods, or other medications prescribed by a healthcare professional.
Key Points:
- Spasmodic dysmenorrhea causes severe and painful menstrual cramps during menstruation
- Muscle spasms in the uterus are a characteristic feature of this condition
- It can cause significant discomfort and may interfere with daily activities
- Treatment options include:
- Over-the-counter pain relievers
- Hormonal birth control
- Other prescribed medications
- OTC pain relievers and hormonal birth control are commonly used to manage symptoms
- A healthcare professional can prescribe other medications to help alleviate symptoms if necessary
spasmodic dysmenorrhea – Watch Video
💡
Pro Tips:
1. Spasmodic dysmenorrhea, also known as menstrual cramps, affects approximately one in five women during their reproductive years.
2. The pain experienced by individuals with spasmodic dysmenorrhea is caused by the uterus contracting excessively during menstruation, leading to intense cramping sensations.
3. Although menstrual cramps are common, severe cases of spasmodic dysmenorrhea can disrupt daily activities and may require medical intervention for pain management.
4. Studies suggest that the release of certain prostaglandins, hormone-like substances, during menstruation plays a significant role in causing the uterine contractions that lead to spasmodic dysmenorrhea.
5. Interestingly, some individuals with spasmodic dysmenorrhea have found relief from their symptoms through alternative therapies such as acupuncture, herbal remedies, or heat therapy.
Introduction To Spasmodic Dysmenorrhea
Spasmodic dysmenorrhea is a condition that affects many women during their menstrual cycles. It is characterized by severe and painful menstrual cramps that can significantly impact a person’s quality of life. These cramps are caused by spasms in the muscles of the uterus, leading to intense discomfort. While some women may experience mild cramps during their periods, spasmodic dysmenorrhea refers to the extreme end of the spectrum, where the pain is debilitating and may interfere with daily activities.
- Spasmodic dysmenorrhea is a condition that causes severe and painful menstrual cramps.
- It is characterized by spasms in the muscles of the uterus.
- The pain can be debilitating and interfere with daily activities.
Causes And Symptoms Of Spasmodic Dysmenorrhea
The cause of spasmodic dysmenorrhea is not fully understood, but several factors may contribute to its development. These factors include:
-
Prostaglandins: Prostaglandins are hormone-like substances released during menstruation to stimulate uterine contractions. Elevated levels of prostaglandins can lead to stronger and more painful contractions, causing spasmodic dysmenorrhea.
-
Uterine abnormalities: Some women may have structural abnormalities in their uterus, such as a tilted uterus or the presence of fibroids, that can contribute to more severe menstrual cramps.
-
Hormonal imbalances: Hormonal imbalances, such as high estrogen levels or low progesterone levels, may also play a role in the development of spasmodic dysmenorrhea.
The symptoms of spasmodic dysmenorrhea can vary from woman to woman and may include:
- Severe lower abdominal pain that radiates to the lower back and thighs.
- Intense cramping that may come in waves or be constant.
- Nausea and vomiting.
- Headaches or dizziness.
- Fatigue and weakness.
- Diarrhea or constipation.
- Difficulty concentrating or focusing.
Understanding Uterine Muscle Spasms
Uterine muscle spasms are the main factor behind spasmodic dysmenorrhea. The uterus is composed of smooth muscle tissue, responsible for contracting and relaxing during menstruation. However, in individuals with spasmodic dysmenorrhea, these contractions become stronger and more intense. The primary cause of these spasms is elevated levels of prostaglandins, which stimulate uterine contractions and result in increased pain and discomfort.
Throughout the menstrual cycle, the uterine lining thickens in preparation for pregnancy. If pregnancy does not occur, the lining sheds, leading to menstrual bleeding. The uterus contracts to aid in expelling the lining, but in individuals with spasmodic dysmenorrhea, these contractions become exaggerated, causing severe pain. Moreover, the excessive muscle contractions can disrupt blood flow to the uterus, further contributing to pain and discomfort.
Impact Of Spasmodic Dysmenorrhea On Daily Life
Spasmodic dysmenorrhea is a condition that can have a significant impact on a woman’s daily life. The intense pain and discomfort associated with this condition often make it challenging for women to carry out their normal activities, such as going to work or school. In fact, some women may even need to take time off during their periods due to the severity of the symptoms.
Moreover, spasmodic dysmenorrhea can also have an adverse effect on a person’s emotional well-being. The constant pain and discomfort can lead to feelings of frustration, anxiety, and mood swings. It is important to note that the pain and discomfort from this condition can also interfere with sleep, further impacting a person’s overall quality of life.
Furthermore, the uncertainty of when these intense cramps will strike can create a sense of apprehension and constant fear of the next menstrual cycle. This fear can add to the emotional burden already placed upon women who suffer from spasmodic dysmenorrhea.
To summarize, spasmodic dysmenorrhea is a condition that causes intense pain and discomfort during menstruation. It can significantly impact a woman’s daily life, making it difficult to carry out normal activities and affecting her emotional well-being. The pain interferes with sleep and also creates a constant fear of when the next menstrual cycle will bring more intense cramps.
- The intense pain and discomfort of spasmodic dysmenorrhea can make it challenging to carry out normal activities.
- Some women may need to take time off during their periods due to the severity of the symptoms.
- Spasmodic dysmenorrhea can affect a person’s emotional well-being, leading to feelings of frustration, anxiety, and mood swings.
- The pain and discomfort can interfere with sleep, further impacting a person’s quality of life.
- The uncertainty of when these intense cramps will strike can create a sense of apprehension and a constant fear of the next menstrual cycle.
“Spasmodic dysmenorrhea is a condition that causes intense pain and discomfort during menstruation.”
Over-The-Counter Pain Relief Options For Menstrual Cramps
Fortunately, there are various over-the-counter pain relief options available to help manage the symptoms of spasmodic dysmenorrhea. These include:
-
Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs, such as ibuprofen and naproxen, can help reduce inflammation and relieve pain. They work by blocking the production of prostaglandins, which are responsible for the uterine contractions that cause cramps.
-
Acetaminophen: Acetaminophen can help relieve pain but does not have the anti-inflammatory effects of NSAIDs. It may be a suitable option for individuals who cannot take NSAIDs due to allergies or other medical conditions.
-
Heat therapy: Applying a heating pad or taking a warm bath can help relax the muscles of the uterus and provide temporary relief from cramps. Heat therapy increases blood flow to the area, which can alleviate pain and reduce muscle spasms.
Hormonal Birth Control Methods For Managing Spasmodic Dysmenorrhea
Hormonal birth control methods are an effective way to manage spasmodic dysmenorrhea.
These methods work by regulating hormone levels and can help decrease the production of prostaglandins, thereby reducing the severity of cramps.
Some hormonal birth control options that may be recommended for managing spasmodic dysmenorrhea include:
-
Combination oral contraceptives: These contain both estrogen and progestin hormones and work by preventing ovulation and thinning the uterine lining. They can help regulate the menstrual cycle and reduce the intensity of cramps.
-
Progestin-only contraceptives: These include the progestin-only pill, the birth control implant, and the hormonal IUD. They work by thickening the cervical mucus and thinning the uterine lining, making it more difficult for sperm to reach the egg and for the egg to implant. These methods can result in lighter periods with less severe cramping.
-
Hormonal patches and injections: These methods also contain progestin hormones and work similarly to combination oral contraceptives. They provide longer-term contraception and can be a suitable option for individuals who prefer less frequent dosing.
Medications For Treating Severe Menstrual Cramps
In some cases, over-the-counter pain relief options and hormonal birth control methods may not provide sufficient relief from spasmodic dysmenorrhea. In such situations, a healthcare professional may prescribe other medications to help manage the condition. These may include:
-
Nonsteroidal anti-inflammatory drugs (NSAIDs): Prescription-strength NSAIDs may be recommended for individuals who do not get enough relief from over-the-counter options. These higher doses can more effectively reduce inflammation and relieve pain.
-
Antispasmodic agents: These medications help relax the smooth muscles of the uterus, reducing the intensity of contractions and alleviating cramps. Examples include dicyclomine and hyoscyamine.
-
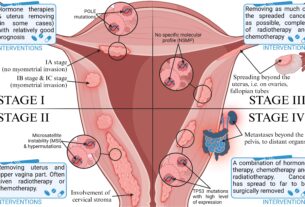
Hormone therapy: In some cases, hormone therapy may be recommended to help regulate hormone levels and reduce the severity of spasmodic dysmenorrhea. This may involve the use of hormones such as progestin or gonadotropin-releasing hormone agonists.
Lifestyle Tips For Coping With Spasmodic Dysmenorrhea
In addition to medical treatments, certain lifestyle changes can also help individuals cope with spasmodic dysmenorrhea. These include:
-
Exercise regularly: Engaging in regular physical activity can help improve blood flow, reduce muscle tension, and alleviate menstrual cramps. Activities such as walking, swimming, or yoga may be beneficial.
-
Practice relaxation techniques: Techniques such as deep breathing, meditation, and mindfulness can help relax the body and reduce stress, which may contribute to muscle tension and worsen symptoms.
-
Apply heat: Applying a heating pad or using a warm compress on the abdomen can help relax the uterine muscles and relieve pain.
-
Dietary changes: Some individuals find that certain dietary changes, such as reducing caffeine and sugar intake, can help reduce the severity of menstrual cramps.
Seeking Medical Attention For Spasmodic Dysmenorrhea
If the symptoms of spasmodic dysmenorrhea are severe or significantly interfere with daily life, it is essential to seek medical attention. A healthcare professional can evaluate the individual’s symptoms, conduct a physical examination, and recommend appropriate treatment options. They may also perform additional tests, such as ultrasound imaging, to rule out any underlying structural abnormalities in the uterus.
- Severe symptoms or significant interference with daily life necessitate medical attention for spasmodic dysmenorrhea.
- Healthcare professionals can evaluate symptoms, conduct physical examinations, and recommend suitable treatment options.
- Additional tests, including ultrasound imaging, may be performed to rule out underlying structural abnormalities in the uterus.
Seeking medical attention is crucial if the symptoms of spasmodic dysmenorrhea are severe or significantly impacting daily life. A healthcare professional will assess symptoms, perform physical examinations, and provide appropriate treatment options. Additional tests, such as ultrasound imaging, may be conducted to rule out any underlying structural abnormalities in the uterus.
Conclusion And Hope For Managing Spasmodic Dysmenorrhea
Spasmodic dysmenorrhea is a challenging and debilitating condition that affects many individuals. Fortunately, there are several treatment options available to help manage its symptoms. Here are some important points to consider:
- Over-the-counter pain relief options can provide temporary relief from menstrual cramps. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen sodium are commonly used for this purpose.
- Hormonal birth control methods, such as birth control pills or the patch, can help regulate hormone levels and reduce the severity of menstrual cramps. These methods work by preventing ovulation and thinning the lining of the uterus.
- In some cases, healthcare professionals may prescribe stronger medication, such as muscle relaxants or prescription pain relievers, to manage the pain associated with spasmodic dysmenorrhea.
- Lifestyle changes can also play a crucial role in managing this condition. Regular exercise, such as low-impact activities like walking or swimming, can help reduce cramping and improve overall well-being.
- Relaxation techniques, such as deep breathing exercises, yoga, or meditation, can help alleviate stress and promote relaxation, which may in turn help reduce the severity of menstrual cramps.
- Heat therapy, such as using a heating pad or taking warm baths, can provide temporary relief from cramping. Applying heat to the lower abdomen can help relax the muscles and ease the pain.
- It is important to work closely with healthcare professionals to determine the best course of treatment for spasmodic dysmenorrhea. They can offer personalized advice and guidance based on individual needs and preferences.
“By working closely with healthcare professionals and exploring different treatment approaches, it is possible to find effective strategies for managing spasmodic dysmenorrhea and improving overall quality of life.”
💡
You may need to know these questions about spasmodic dysmenorrhea
How do you treat spasmodic dysmenorrhea?
One way to treat spasmodic dysmenorrhea is by using nonsteroidal anti-inflammatory drugs (NSAIDs). These medications, such as ibuprofen or naproxen, are readily available over the counter at drug or grocery stores. NSAIDs work by reducing inflammation and relieving pain, making them an effective treatment option for dysmenorrhea. It is important to follow the recommended dosage and guidelines provided by a healthcare professional to ensure proper usage and maximum benefits.
What is dysmenorrhea types spasmodic and congestive?
Dysmenorrhea can manifest in two distinct types: spasmodic and congestive. Spasmodic dysmenorrhea refers to the sharp and intense pelvic cramps experienced at the onset of menstrual flow. These spasms can cause significant discomfort and may vary in intensity from woman to woman. On the other hand, congestive dysmenorrhea is characterized by a deep and dull ache in the pelvic region during menstruation. Unlike spasmodic dysmenorrhea, the pain in congestive dysmenorrhea tends to be more persistent and consistent throughout the menstrual period. Understanding the type of dysmenorrhea can help in identifying the most appropriate management and treatment options for individuals experiencing menstrual pain.
What is the difference between menstrual cramps and dysmenorrhea?
Menstrual cramps and dysmenorrhea are terms used to describe different levels of pain during menstruation. Menstrual cramps refer to the normal discomfort experienced by many women during their periods. These cramps typically involve mild to moderate pain and are often felt as a tightening or cramping sensation in the pelvic region. On the other hand, dysmenorrhea refers to more severe and debilitating period pain. It involves intense cramping in the pelvic area, but can also be accompanied by pain in the stomach, lower back, and legs. Unlike ordinary menstrual cramps, dysmenorrhea can be constant and persistent, causing a prolonged and persistent ache.
How serious is dysmenorrhea?
Dysmenorrhea, the pain associated with menstruation, can vary in seriousness from mild to severe. While more than half of menstruating women experience some level of pain for a day or two each month, for certain individuals, the pain can be debilitating, disrupting their daily activities for several days. This severe form of dysmenorrhea significantly impacts these women’s quality of life, highlighting the importance of addressing this issue and finding effective ways to manage and alleviate the pain.
Reference source
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8943241/
https://my.clevelandclinic.org/health/diseases/4148-dysmenorrhea
https://www.hopkinsmedicine.org/health/conditions-and-diseases/dysmenorrhea
https://medbroadcast.com/condition/getcondition/dysmenorrhea