Embarrassing situations can strike at the most inconvenient moments – a sneeze, a hearty laugh, or even a sudden movement.
If you’ve ever experienced the embarrassing mishap of stress incontinence – the unintentional loss of urine due to physical activity or bladder pressure – fear not!
Discover the myriad of treatment options available, from pelvic floor exercises to surgical procedures, and take charge of your life again.
But remember, consulting with a healthcare provider is key to finding the best approach for your unique needs.
Now, let’s dive into the world of stress incontinence and regain control!
stress incontinence
Stress incontinence refers to the unintentional loss of urine that occurs when pressure is exerted on the bladder during physical movement or activity.
It is more common in women than men and is characterized by weakened muscles that control the release of urine in the urinary sphincter.
Common causes include childbirth and prostate surgery, while factors such as chronic coughing, obesity, smoking, and high-impact activities can worsen symptoms.
Diagnosis involves a medical history, physical exam, urine sample, and specialized tests, and treatment options include pelvic floor exercises, lifestyle changes, devices, and surgical procedures.
It is important to seek medical advice and support to determine the most suitable treatment for stress incontinence.
Key Points:
- Stress incontinence is the unintentional loss of urine caused by pressure on the bladder during physical movement or activity.
- It is more common in women and is characterized by weakened muscles in the urinary sphincter.
- Common causes include childbirth and prostate surgery, while factors like chronic coughing, obesity, smoking, and high-impact activities can worsen symptoms.
- Diagnosis involves a medical history, physical exam, urine sample, and specialized tests.
- Treatment options include pelvic floor exercises, lifestyle changes, devices, and surgical procedures.
- Seeking medical advice and support is important to determine the most suitable treatment for stress incontinence.
stress incontinence – Watch Video
💡
Pro Tips:
1. Stress incontinence, a common condition primarily affecting women, is characterized by the involuntary leakage of urine during physical activities such as coughing, sneezing, laughing, or exercising.
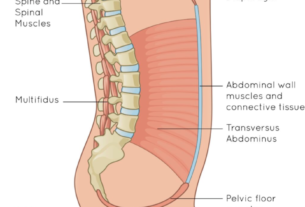
2. Contrary to popular belief, stress incontinence is not solely caused by psychological stress. It is primarily the result of weakened pelvic floor muscles that support the bladder and urethra, leading to urinary leakage.
3. Pelvic floor exercises, commonly known as Kegel exercises, can greatly help in managing and reducing stress incontinence. These exercises aim to strengthen the muscles responsible for controlling urine flow, and can be easily performed at home without any equipment.
4. Obesity has been identified as one of the risk factors associated with stress incontinence. Excess weight places additional pressure on the bladder and pelvic floor muscles, making them more susceptible to weakness and causing urine leakage.
5. While stress incontinence is more common in women, it can also affect men. In men, stress incontinence is often a result of prostate surgery, which may damage the muscles and nerves involved in bladder control. Proper rehabilitation and targeted exercises are essential for restoring urinary continence in these cases.
Definition and Causes of Stress Incontinence
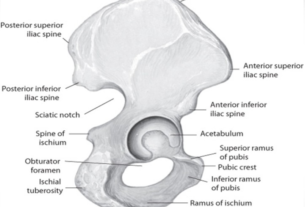
Stress incontinence is a common condition characterized by the unintentional loss of urine. It occurs when physical movement or activity puts pressure on the bladder, causing urine leakage. This condition is more prevalent in women than men. The weakening of the muscles that control the release of urine in the urinary sphincter is a key characteristic of stress incontinence. When abdominal and pelvic muscles are exerted through actions such as coughing, sneezing, bending over, lifting heavy objects, or laughing hard, urine leakage may occur.
The causes of weakened pelvic floor muscles and urinary sphincter vary, but common factors include childbirth and prostate surgery. Women who have given birth vaginally and men who have undergone surgery for prostate cancer are at a higher risk of developing stress incontinence. Additionally, chronic coughing, obesity, smoking, and engaging in high-impact activities can worsen stress incontinence.
- Weak pelvic floor muscles and urinary sphincter
- Childbirth and prostate surgery are common causes
- Higher risk for women who have given birth vaginally and men who have undergone prostate surgery
- Chronic coughing, obesity, smoking, and high-impact activities can worsen stress incontinence.
Symptoms and Risk Factors for Stress Incontinence
The symptoms of stress incontinence are often observed during physical activities that put pressure on the bladder. Common symptoms include:
- Leaking urine when coughing, sneezing, laughing, bending over, lifting something heavy, or during exercise or sexual activity.
Risk factors for developing stress incontinence include:
- Age
- Type of childbirth delivery (vaginal delivery increases the risk)
- Body weight (overweight or obese individuals have a higher risk)
- Previous pelvic surgery (such as a hysterectomy in women or surgery for prostate cancer in men).
Note: Stress incontinence refers to the involuntary leakage of urine during physical activities that put pressure on the bladder.
Diagnosis of Stress Incontinence
Diagnosing urinary stress incontinence involves a variety of medical evaluations, including:
- Thorough medical history assessment
- Physical examination
- Urine sample analysis
- Neurological examination
In some cases, additional tests may be ordered to further evaluate bladder function, such as:
- Measurements of post-void residual urine
- Cystometry to measure bladder pressures
- Video urodynamics to create images of the bladder
- Cystoscopy to identify any potential blockages or abnormalities in the bladder and urethra
It is important to discuss the results of these tests with a healthcare provider to determine the most appropriate treatment strategy.
Treatment Strategies for Stress Incontinence
Fortunately, stress incontinence can often be effectively managed with various treatment strategies. One of the key approaches is performing pelvic floor muscle exercises, commonly known as Kegel exercises. These exercises can strengthen the pelvic floor muscles, improving their ability to control the release of urine. Additionally, managing fluid consumption, adopting a healthy lifestyle (such as quitting smoking, losing weight, and treating chronic cough), and bladder training techniques can help alleviate the symptoms of stress incontinence.
Medication and Device Options for Stress Incontinence
Currently, there are no approved medications in the United States specifically designed for treating stress incontinence. However, in Europe, the antidepressant duloxetine is used to manage this condition. In some cases, healthcare providers may recommend the use of devices to help control stress incontinence.
- Vaginal pessaries
- Urethral inserts
are two common options for women. Inserts are particularly suitable for activities such as heavy lifting, running, or playing tennis, where urine leakage may be more likely.
It is important to consult with a healthcare professional to determine the most appropriate treatment options for stress incontinence.
Surgical Procedures for Stress Incontinence
For individuals with more severe cases of stress incontinence, surgical procedures may be considered. Some of the surgical options available include:
- Burch procedure: This procedure involves the use of sutures to support the bladder neck and urethra.
- Sling procedure: The sling procedure is the most common surgical intervention for women with stress urinary incontinence, but it can also be used for men. It involves the placement of a sling to support the urethra and improve bladder control.
- Injectable bulking agents: This option involves injecting synthetic materials to bulk up the area around the urethra, improving the closing ability of the sphincter.
- Retropubic colposuspension: This procedure entails sutures attached to ligaments along the pubic bone to lift and support tissues near the bladder neck and urethra.
- Inflatable artificial sphincter: In men, this is a surgically implanted device that replaces the function of the sphincter.
These surgical procedures offer effective solutions for individuals with severe stress incontinence. They aim to improve bladder control and minimize involuntary leakage of urine.
Lifestyle Practices for Managing Stress Incontinence
In addition to medical interventions, certain lifestyle practices can help manage stress incontinence. Some ways to do this include:
- Shedding extra weight: Losing weight can alleviate symptoms of stress incontinence.
- Incorporating high-fiber foods: Including whole grains, legumes, fruits, and vegetables in your diet can relieve and prevent constipation, which can contribute to urinary incontinence.
- Avoiding irritants: It is advisable to avoid certain foods and beverages like chocolate, coffee, tea, and carbonated beverages, as these can irritate the bladder and potentially worsen urinary leakage.
- Quitting smoking: Smoking is another factor that can worsen the symptoms of stress incontinence and is associated with a higher risk of bladder cancer.
To summarize, managing stress incontinence involves incorporating healthy lifestyle choices such as weight loss, a high-fiber diet, avoiding bladder irritants, and quitting smoking.
Coping Strategies for Intimacy and Sexual Activity
Stress incontinence can have an impact on sexual activity, but there are strategies that can help manage this issue. Open communication with your partner is crucial in dealing with urine leakage during sexual intercourse. It is important to be honest about your symptoms and work together to find positions or techniques that are comfortable and can reduce the occurrence of leakage.
In addition, emptying the bladder before intimacy and avoiding fluid intake beforehand can also help lessen the likelihood of leakage. Finally, one technique that can be beneficial is for the woman to be on top during sex, as this allows better control of the pelvic muscles and can help minimize the risk of urine leakage.
To summarize, here are some strategies to manage stress incontinence during sexual activity:
- Open communication with your partner
- Honest discussion about symptoms
- Exploring comfortable positions and techniques
- Emptying the bladder before intimacy
- Avoiding fluid intake beforehand
- Trying the woman on top position during sex
“Open communication is key to managing stress incontinence during sexual activity.”
Seeking Support and Resources for Stress Incontinence
Dealing with stress incontinence can be emotionally challenging, and finding support is essential. Support groups can provide opportunities to voice concerns and obtain motivation for self-care strategies. It is important to find a healthcare provider who specializes in this field and can work with you to determine the best treatment options for your incontinence. They can provide guidance and resources to help you manage your condition effectively.
- Finding support is essential in dealing with stress incontinence
- Support groups offer opportunities to voice concerns and obtain motivation
- Find a healthcare provider who specializes in this field to determine the best treatment options for your incontinence
- A healthcare provider can provide guidance and resources to effectively manage the condition.
Tips for Healthcare Appointments and Communications
When seeking medical assistance for stress incontinence, preparation is key. It is helpful to be prepared for healthcare appointments by filling out a questionnaire and keeping a bladder diary to track symptoms and triggers. Additionally, specialized testing may require a referral to a urologist or urogynecologist. To ensure effective communication, it is important to provide your healthcare provider with a comprehensive list of symptoms and any medications, herbs, or vitamin supplements you are taking. Open and honest communication with your healthcare provider will facilitate the development of an appropriate treatment plan.
💡
You may need to know these questions about stress incontinence
What is the major cause of stress incontinence?
The major cause of stress incontinence is weakened pelvic muscles, which can occur as a result of childbirth. During childbirth, the pelvic muscles can stretch and sometimes become damaged, leading to a loss of strength and support for the urethra. This can result in the bladder or other organs dropping and placing pressure on the urethra, causing stress incontinence. Other factors, such as aging, hormonal changes, and certain medical conditions, can also contribute to the weakened pelvic muscles, further exacerbating the condition of stress incontinence.
Can you fix stress urinary incontinence?
Yes, stress urinary incontinence can be treated. One option is through behavior changes and bladder training, where individuals learn techniques to control their bladder and minimize leakage. Another approach is pelvic floor muscle training, which involves exercises that strengthen the muscles responsible for bladder control. If these methods do not provide sufficient relief, surgery may be considered as a more permanent solution to address stress urinary incontinence.
What are the 4 types of incontinence?
There are four distinct types of urinary incontinence: urgency, stress, functional, and overflow incontinence. Urgency incontinence occurs when there is a sudden and uncontrollable urge to urinate, leading to involuntary leakage. Stress incontinence refers to the inability to hold urine due to pressure on the bladder caused by physical activities such as sneezing, coughing, or exercising. Functional incontinence occurs when a person has a physical or mental impairment that prevents them from reaching the toilet in time. Lastly, overflow incontinence happens when the bladder does not empty completely, causing it to frequently overflow. Various treatment options like behavioral therapies, medications, nerve stimulation, and surgery can help manage and alleviate the symptoms of urinary incontinence.
What is the best medication for stress incontinence?
One potential medication for stress incontinence is Mirabegron. Mirabegron is a beta-3 adrenergic agonist that relaxes the bladder muscles, increasing the bladder capacity and reducing the frequency of leaks. While it is generally well-tolerated, it is necessary to consult with a healthcare professional to determine the appropriate dosage and potential side effects. In addition to medication, lifestyle modifications and pelvic floor exercises may also be beneficial in managing stress incontinence.
Reference source
https://www.ncbi.nlm.nih.gov/books/NBK539769/
https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/stress-urinary-incontinence
https://www.mayoclinic.org/diseases-conditions/stress-incontinence/diagnosis-treatment/drc-20355732
https://www.mountsinai.org/health-library/diseases-conditions/stress-urinary-incontinence