Anovulatory Functional Bleeding: Causes, Symptoms, and Treatment Explained
– Anovulatory functional bleeding is a condition characterized by irregular or heavy bleeding without ovulation.
– Treatment options for anovulatory functional bleeding include combination oral contraceptives, medroxyprogesterone acetate, megestrol, and levonorgestrel-releasing intrauterine systems.
– Combination oral contraceptives with ≤35 mcg of ethinyl estradiol are effective for contraception but are contraindicated in certain individuals with specific medical conditions.
– Medroxyprogesterone acetate and megestrol do not provide contraception and caution is advised in patients with severe hepatic dysfunction.
– Levonorgestrel-releasing intrauterine systems provide contraception for five years and may cause irregular bleeding or amenorrhea. They are contraindicated in patients with breast cancer, uterine anomalies, acute pelvic or cervical infection, and severe cirrhosis or liver cancer.
– Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, naproxen sodium, and mefenamic acid can be used to treat dysmenorrhea associated with anovulatory bleeding.
– Tranexamic acid is an option approved by the FDA for menorrhagia associated with anovulatory functional bleeding, but caution is advised in patients with a history or risk of thromboembolic or renal disease. It is contraindicated in patients with active intravascular clotting or subarachnoid hemorrhage.
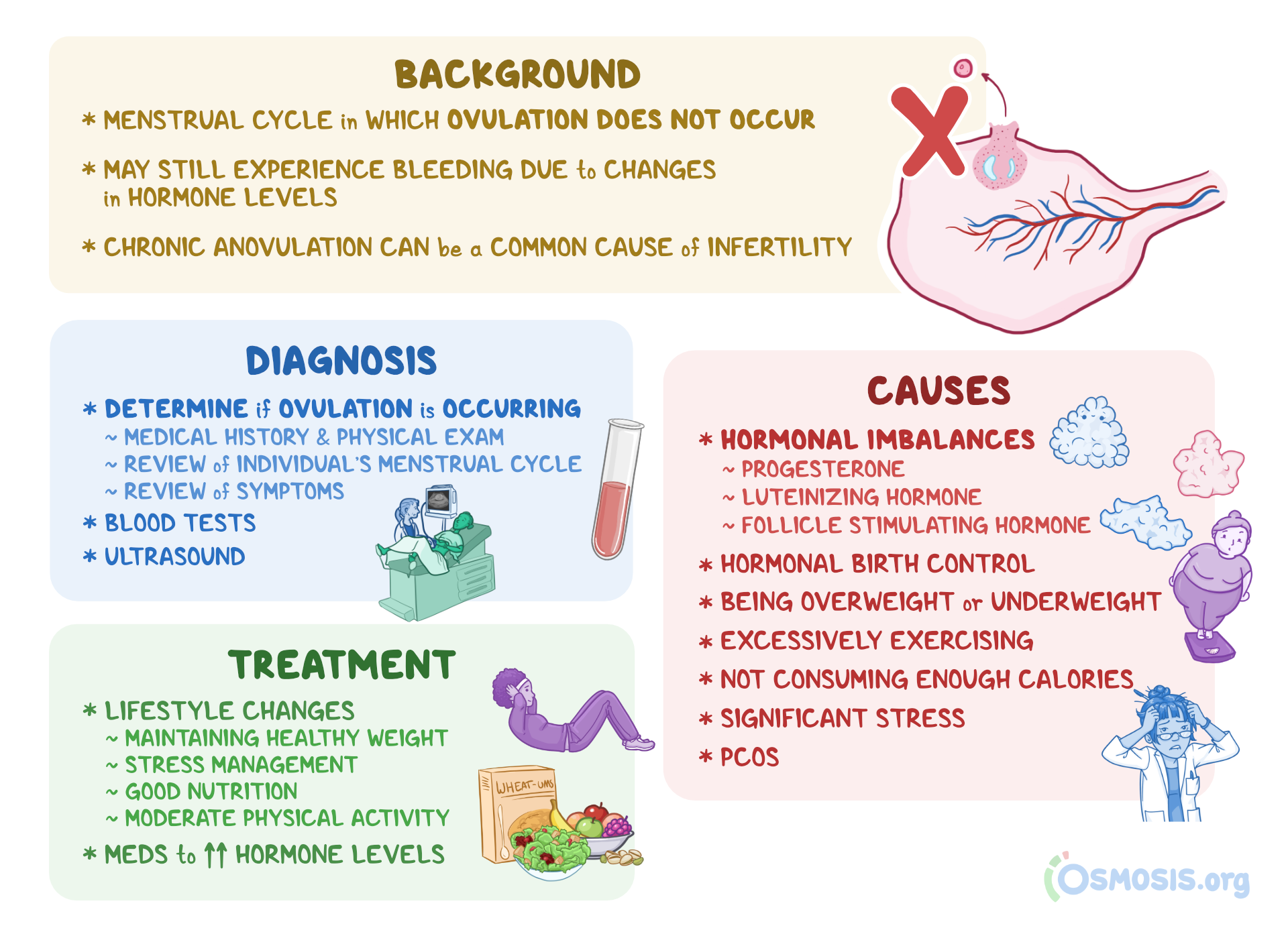
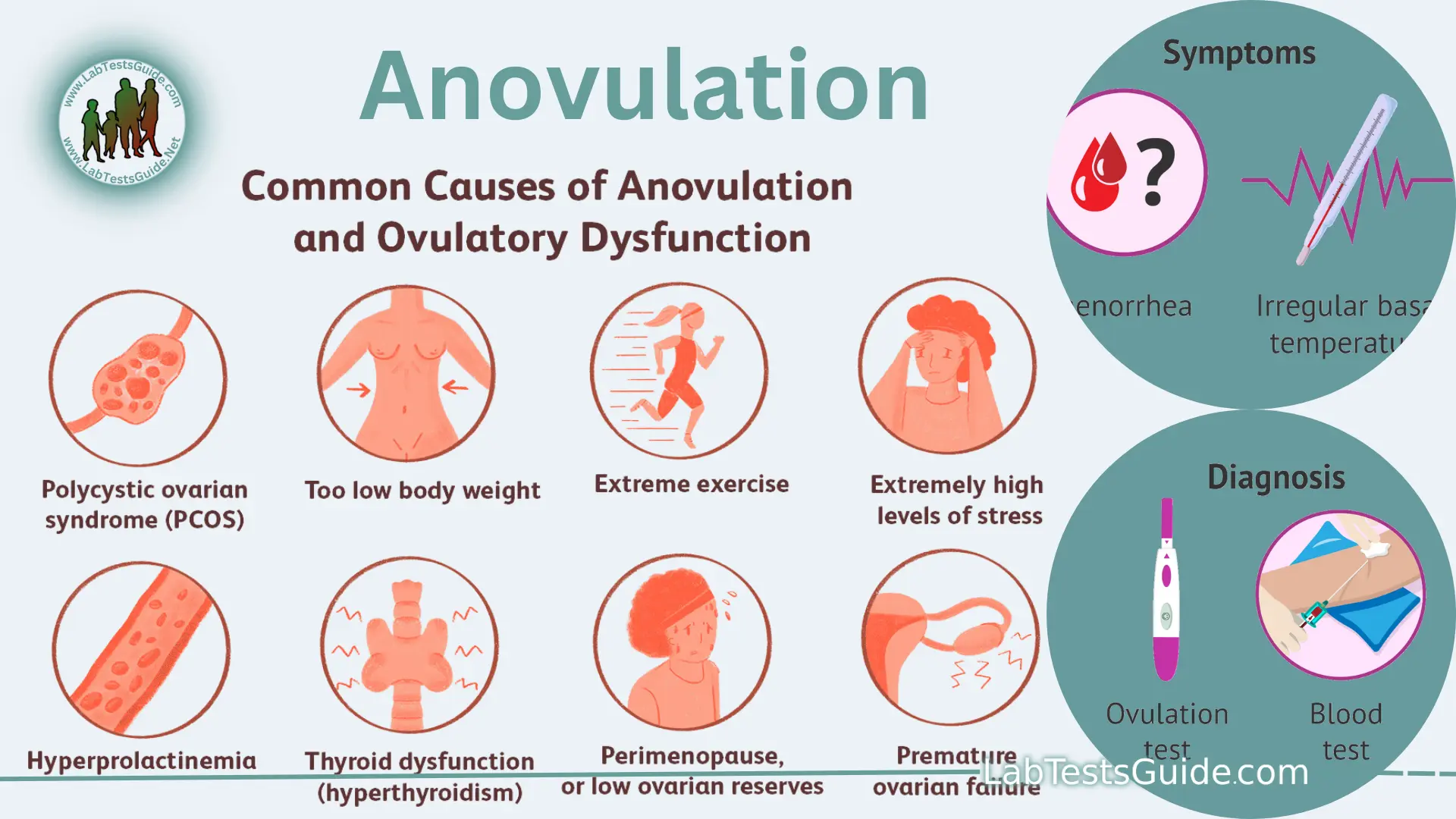
– Anovulatory bleeding is a type of abnormal uterine bleeding that occurs when ovulation does not happen.
– Anovulation can be caused by physical or psychological stressors and is common for women to experience an occasional anovulatory cycle.
– Chronic anovulation can lead to the lining of the uterus building up without being shed, resulting in irregular and potentially heavier bleeding.
– Causes of anovulatory bleeding can include hormonal imbalances during adolescence and the perimenopausal transition, as well as obesity.
– Treatment options for anovulatory bleeding typically involve hormonal methods such as the oral contraceptive pill or progestin-containing IUD.
– Weight loss is important for obese individuals experiencing anovulatory bleeding. Medical advice should be sought if there are concerns about irregular bleeding or menstrual cycle issues.