Syphilis: History, Symptoms, Treatment, and Prevention Explained
– Syphilis is a sexually transmitted infection (STI) that can cause serious health problems without treatment.
– Syphilis is spread through direct contact with a syphilis sore during vaginal, anal, or oral sex, and can also be transmitted from a mother with syphilis to her unborn baby.
– Syphilis cannot be spread through casual contact with objects like toilet seats or doorknobs.
– To reduce the risk of getting syphilis, one can abstain from sex or be in a long-term mutually monogamous relationship with a partner who has been tested and does not have syphilis. Using condoms correctly every time during sex can also help prevent transmission.
– People at risk for syphilis include sexually active individuals without condom use with a partner who has syphilis, gay or bisexual men, individuals with HIV, those taking pre-exposure prophylaxis (PrEP) for HIV prevention, and those with partners who have tested positive for syphilis.
– Pregnant people should be tested for syphilis at their first prenatal visit, and some may need additional testing during the third trimester and at delivery.
– Untreated syphilis during pregnancy can result in low birth weight, premature birth, stillbirth, and serious health problems such as cataracts, deafness, seizures, and death for the baby.
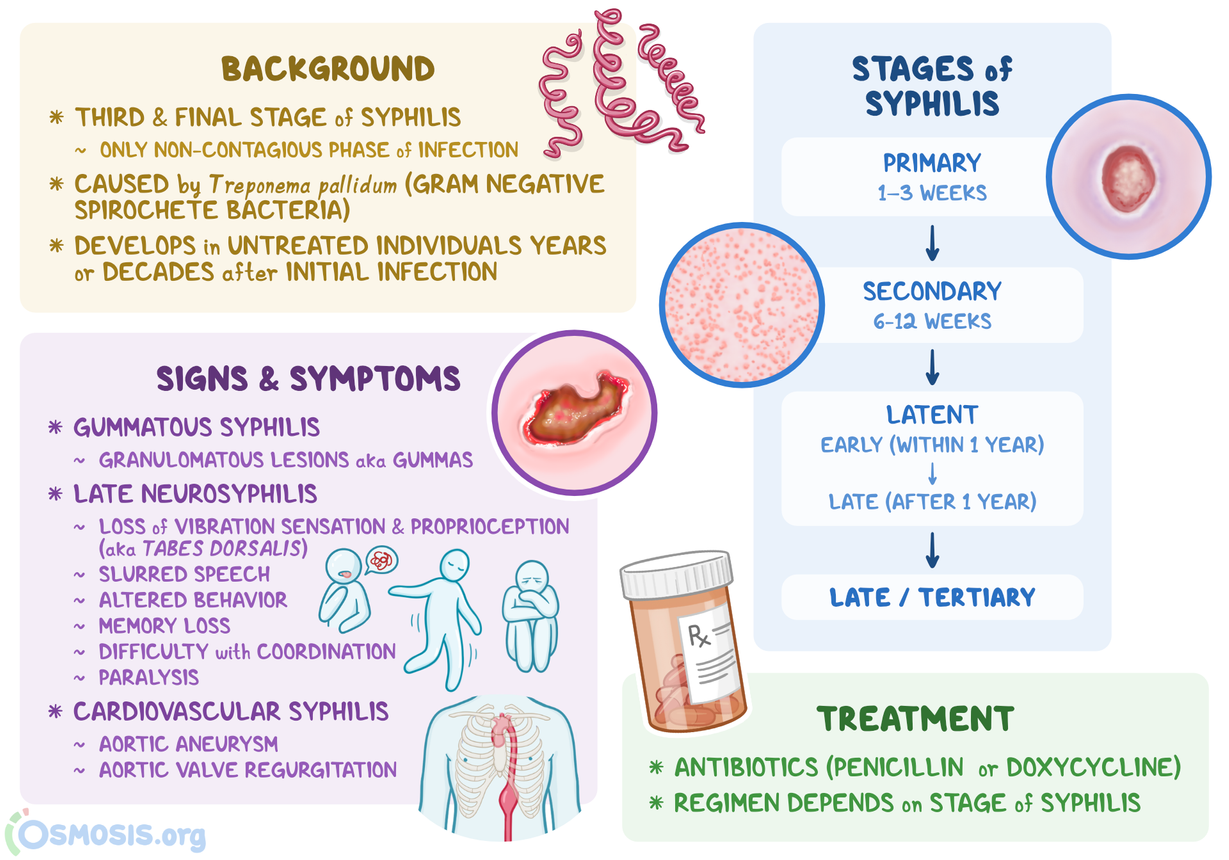
– Syphilis has four stages (primary, secondary, latent, and tertiary) and each stage has different signs and symptoms.
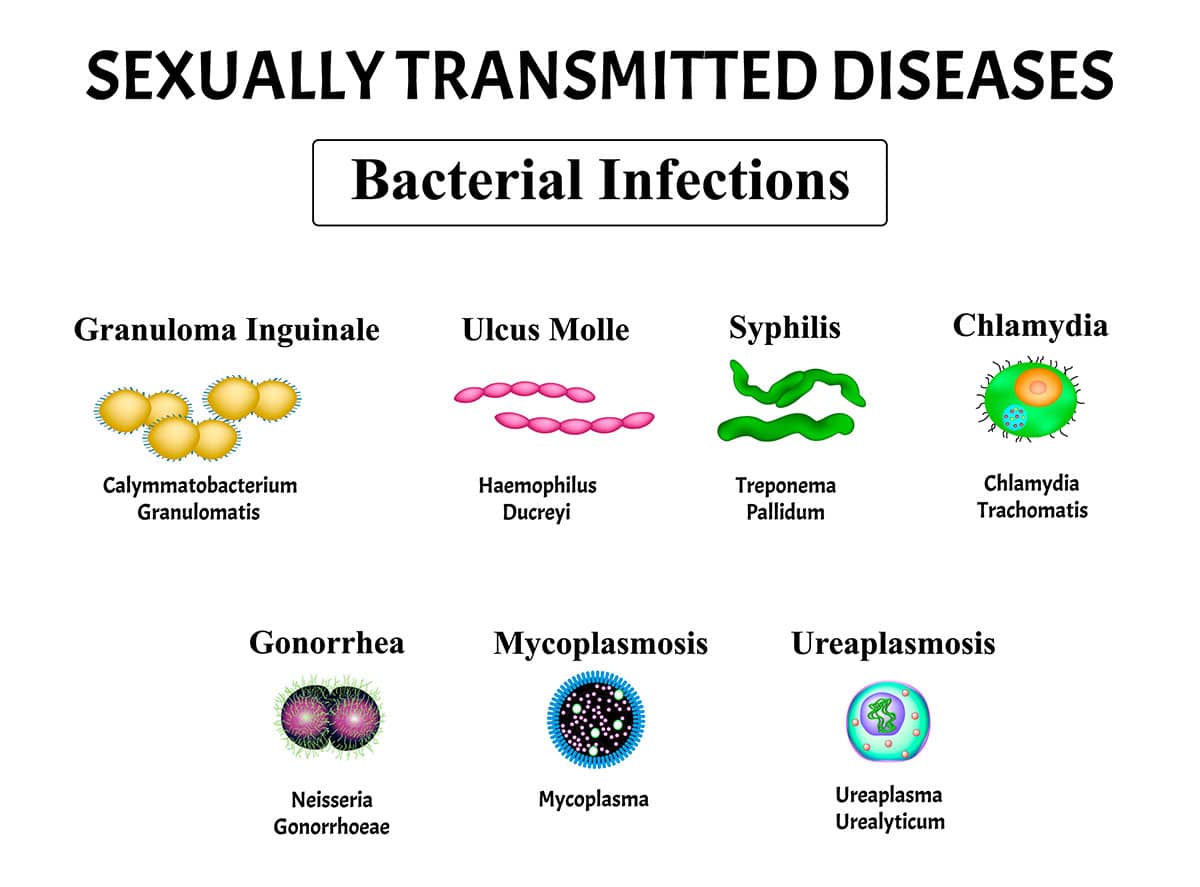
– Syphilis is a sexually transmitted infection caused by the bacterium Treponema pallidum.
– Symptoms of syphilis may include painless sores on or around the genitals, anus, mouth, lips, or rectum.
– The secondary stage of syphilis can involve skin rashes and sores in the mouth, vagina, or anus.
– During the latent stage, there are no visible signs or symptoms of syphilis, but the infection persists in the body.
– Without treatment, syphilis can progress to tertiary stage, affecting various organ systems, including the heart, blood vessels, brain, and nervous system.
– Tertiary syphilis can cause serious damage to internal organs and potentially lead to death.
– Syphilis can spread to the brain and nervous system (neurosyphilis), the eye (ocular syphilis), or the ear (otosyphilis).
– Neurosyphilis may cause severe headaches, muscle weakness, changes in mental state, and dementia.
– Ocular syphilis can lead to eye pain, redness, vision changes, or blindness.
– Otosyphilis may cause hearing loss, tinnitus (ringing in the ears), and dizziness or vertigo.
– Syphilis can be diagnosed through blood tests or by testing fluid from a syphilis sore.
– Treatment for syphilis is necessary to prevent the infection from progressing and may not undo any damage caused by the infection.
– Receiving treatment for syphilis does not protect against getting it again.
– Laboratory tests are necessary to confirm the presence of syphilis.
– Follow-up testing by a healthcare provider is needed to ensure the success of treatment.
– Syphilis sores can be difficult to see in certain areas such as the vagina, anus, mouth, or under the foreskin.
– Getting syphilis again is possible if sex partners do not receive testing and treatment.