Partial Placenta Praevia: Causes, Symptoms, and Management Strategies
List:
– Placenta previa
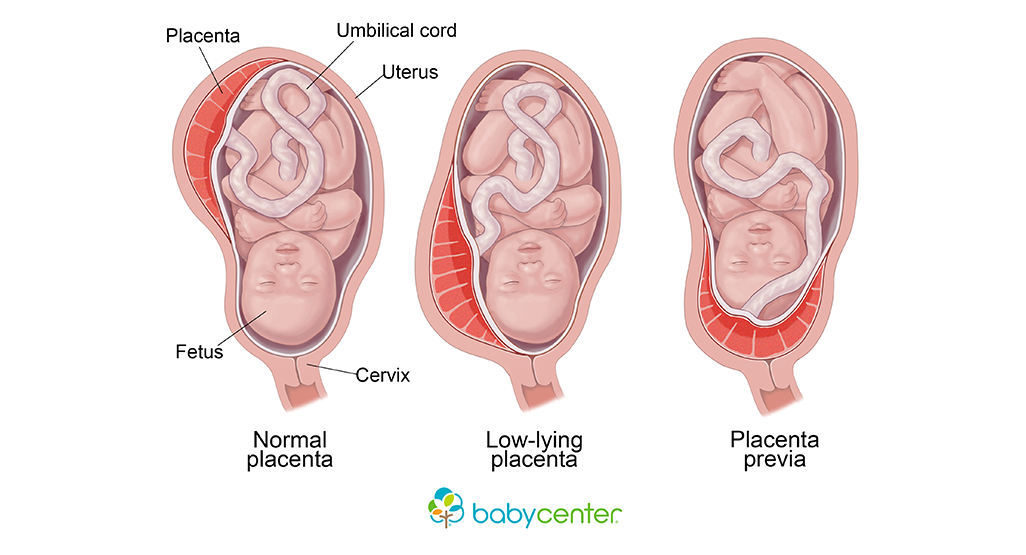
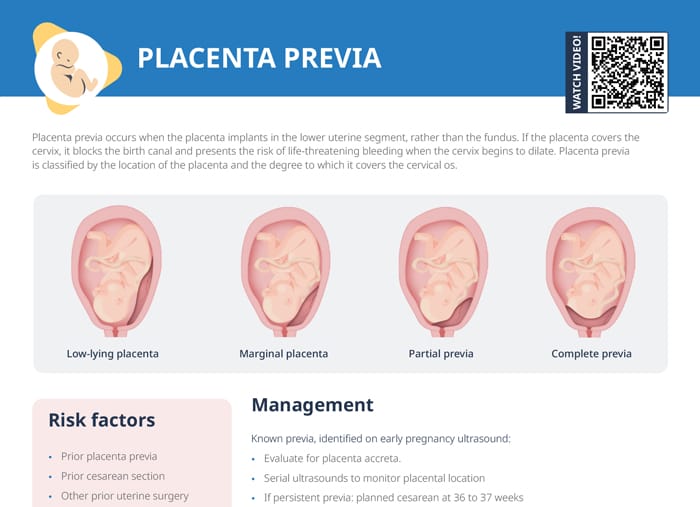
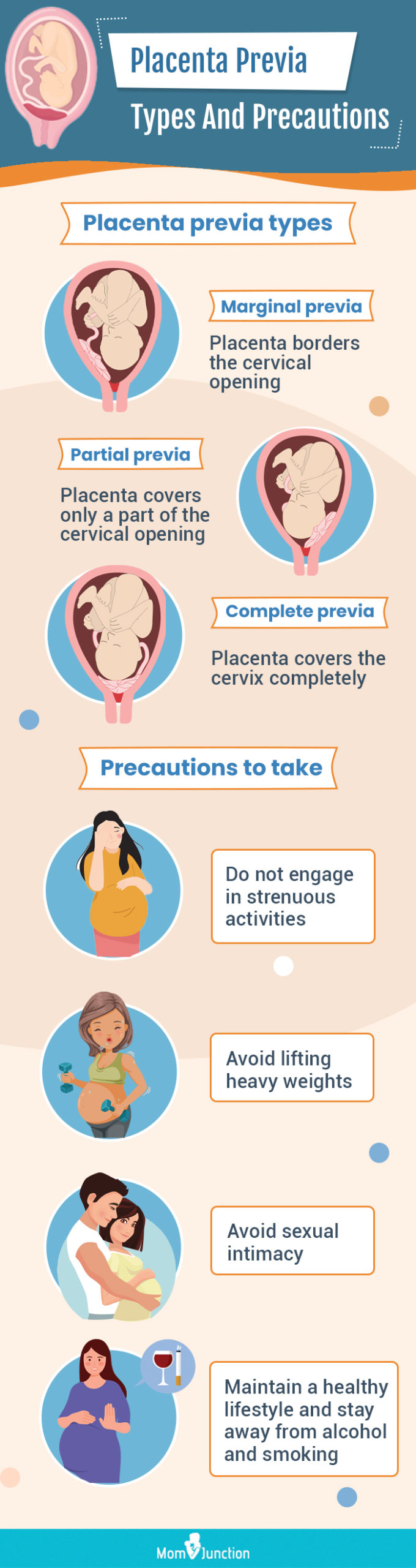
– Condition where the placenta implants at the bottom of the uterus, covering the cervix
– Painless vaginal bleeding after 20 weeks of pregnancy
– 1 in every 200 pregnancies affected by placenta previa
– Other causes of vaginal bleeding during pregnancy
– Thinning and spreading of the bottom part of the uterus can cause bleeding if the placenta is anchored to the bottom
– Sexual intercourse can cause bleeding
– Complications of placenta previa: major bleeding, shock, fetal distress, premature labor or delivery, health risks to the baby, emergency cesarean delivery, hysterectomy, blood loss for the baby, and death
– Causes and risk factors for placenta previa: low implantation of the fertilized egg, abnormalities of the uterine lining, scarring of the uterine lining, abnormalities of the placenta, and multiple pregnancies
– Tests used to diagnose placenta previa: ultrasound scans, feeling the mother’s belly
– Differentiating between placenta previa and placental abruption
– Life-threatening condition for both the mother and baby
– Diagnosis involves ultrasound scan and gentle speculum vaginal examination
– Treatment options depend on factors: type and location of the placenta, amount of blood loss, gestational age of the baby, and the health of both the baby and mother
– Medical treatment during pregnancy: bed rest, hospitalization, close monitoring, blood transfusion, avoiding activities that trigger contractions
– Delivery usually done through a caesarean section
– Postpartum monitoring for complications such as postpartum bleeding
– Baby closely monitored for health issues related to prematurity or lack of oxygen during delivery
– Prompt medical attention needed if experiencing vaginal bleeding during pregnancy
– Treatment options depend on factors such as the type and location of the placenta, amount of blood lost, gestational age of the baby, and the health of both the baby and mother
– Treatment during pregnancy may include bed rest, hospitalization, close monitoring, blood transfusion, and avoiding activities that trigger contractions
– Caesarean section usually performed once the baby is old enough
– Tests to check the mother’s blood cell counts and clotting ability needed.