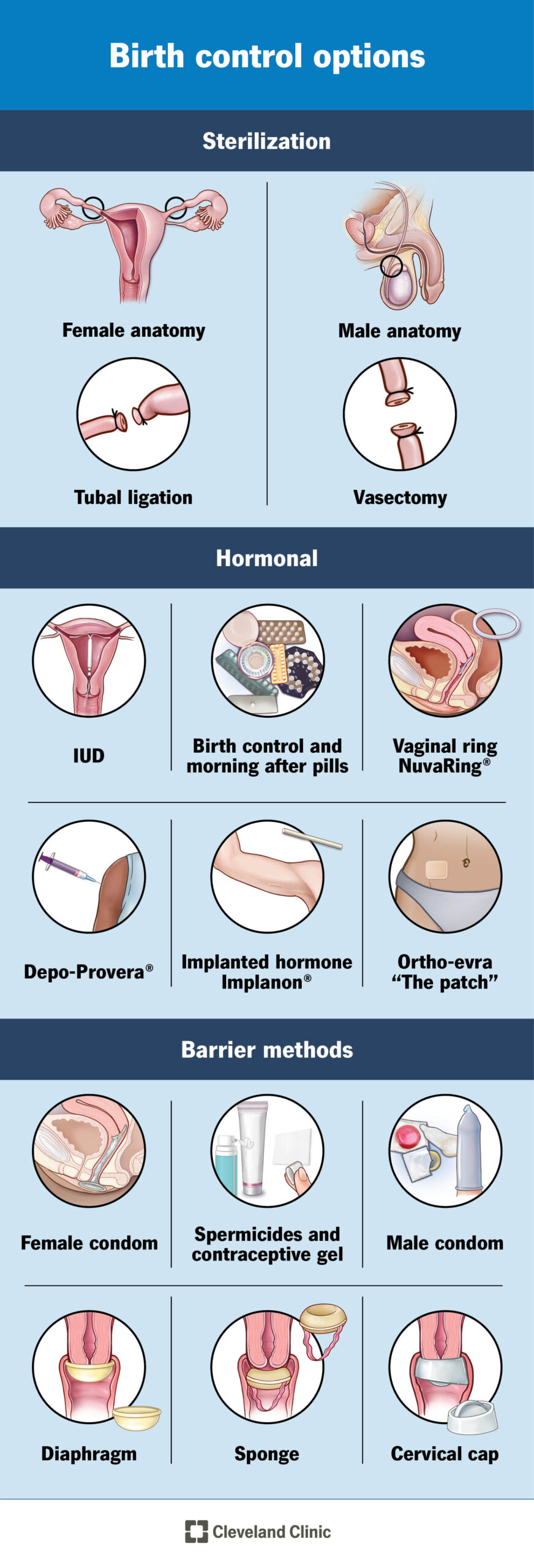
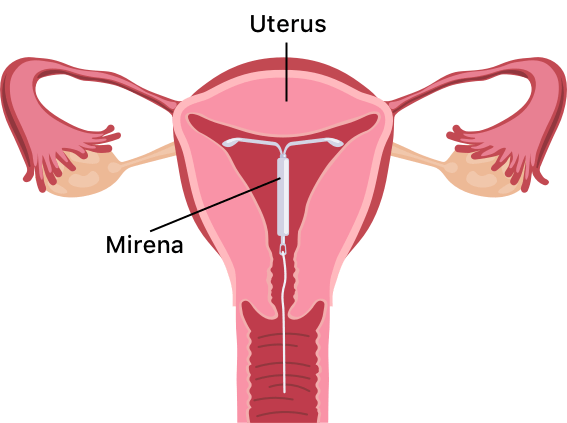
– An IUD is a small T-shaped plastic and copper device that is inserted into the uterus to prevent pregnancy.
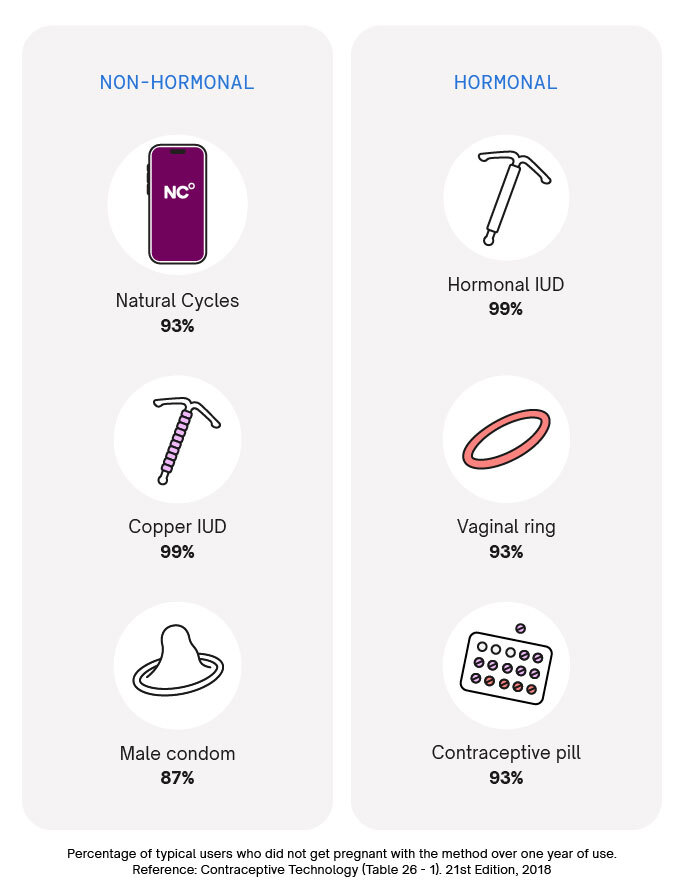
– When inserted correctly, IUDs are more than 99% effective.
– The IUD releases copper into the womb, altering cervical mucus to make it difficult for sperm to reach an egg and survive.
– It can also prevent a fertilized egg from implanting.
– The IUD can be left in for between 5 and 10 years, depending on the type.
– It can be inserted at any time during the menstrual cycle as long as the person is not pregnant.
– It can be taken out at any time by a trained doctor or nurse, and pregnancy is possible immediately after removal.
– Side effects include potentially heavier, longer, or more painful periods in the first 3 to 6 months, as well as spotting or bleeding between periods.
– There is a small risk of infection or the IUD being pushed out or moved.
– Painkillers can be taken after insertion to manage discomfort.
– It may not be suitable for individuals with previous pelvic infections.
– The IUD does not protect against sexually transmitted infections, so additional methods like condoms may be necessary.
– If an IUD is fitted at age 40 or older, it can be left in until menopause or no longer needing contraception.
– Before insertion, a healthcare professional will check the position and size of the womb and may test for infections and provide antibiotics.
– The fitting process takes about 20 to 30 minutes, with the IUD insertion itself taking around 5 minutes. Local anesthesia can be used for comfort.
– After having an IUD fitted, you may experience period-type cramps and bleeding for a few days.
– It is advised to get the IUD checked by a GP after 3 to 6 weeks.
– Issues such as pain in the lower abdomen, high temperature, or abnormal discharge may indicate an infection.
– An IUD has two thin threads that hang down from the womb into the vagina, and they can be checked to ensure the IUD is in place.
– If the threads cannot be felt or if the IUD has moved, additional contraception should be used and a GP or nurse should be consulted.
– An IUD can be removed by a trained doctor or nurse at any time.
– Additional contraception should be used for 7 days before removing the IUD if not getting another one.
– Most people with a womb can use an IUD, but it may not be suitable for those who are pregnant, have an untreated STI, or have womb or cervix problems.
– Those who have had an ectopic pregnancy or have an artificial heart valve should consult their GP before getting an IUD.
– An IUD can usually be fitted 4 weeks after giving birth, and alternative contraception should be used until then.
– An IUD can be used immediately after giving birth, and it will not affect milk supply.
– An IUD can be fitted immediately after an abortion or miscarriage, providing immediate protection against pregnancy.
– Advantages of using an IUD include long-term pregnancy prevention (5 or 10 years depending on the type), immediate effectiveness, no hormonal side effects, and no interruption of sex.
– Disadvantages of using an IUD include the possibility of heavier, longer, or more painful periods, lack of protection against STIs requiring the use of additional condoms, potential for pelvic infections if not treated, and the possibility of vaginal bleeding and pain.
– Risks of using an IUD include a small chance of pelvic infection within 20 days of insertion, slightly higher chance of recurring thrush, potential rejection or displacement of the IUD by the womb, and rare cases of the IUD making a hole in the womb.
– If an IUD fails and pregnancy occurs, there is a risk of ectopic pregnancy.
– An IUD can be obtained for free from contraception clinics, sexual health or genitourinary medicine clinics, GP surgeries, and some young people’s services.
– Contraception services are free and confidential for individuals under the age of 16.
– If a person under 16 wants contraception, the healthcare professional will not inform their parents or carer as long as they believe the individual fully understands the information and decisions being made.
– Doctors and nurses only disclose information if they believe the individual is at risk of harm, such as abuse.
Continue Reading