Fetal Breath Movement: Understanding Its Significance During Development
Here is the updated list of pertinent information related to the keyword “fetal breath movement” without any duplication:
– Babies don’t breathe in the womb in the traditional sense as they don’t have access to air.
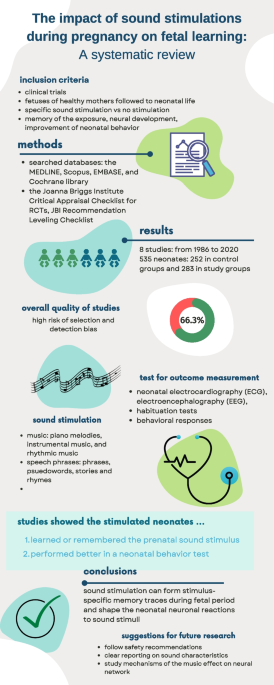
– They practice breathing movements called fetal breathing movements.
– Fetal breathing movements help strengthen the muscles involved in breathing and may support the development of air sacs in the lungs.
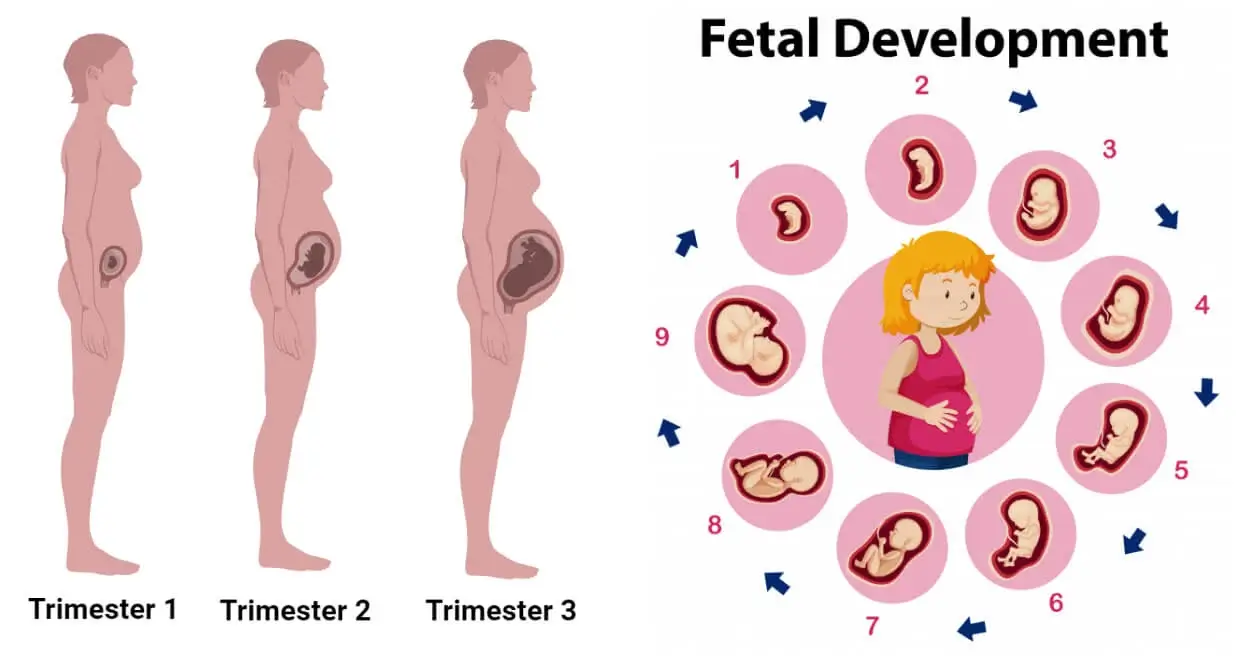
– These movements start around week 10 of pregnancy but become more frequent after week 20.
– Fetal breathing movements are not necessary for survival and may not happen constantly.
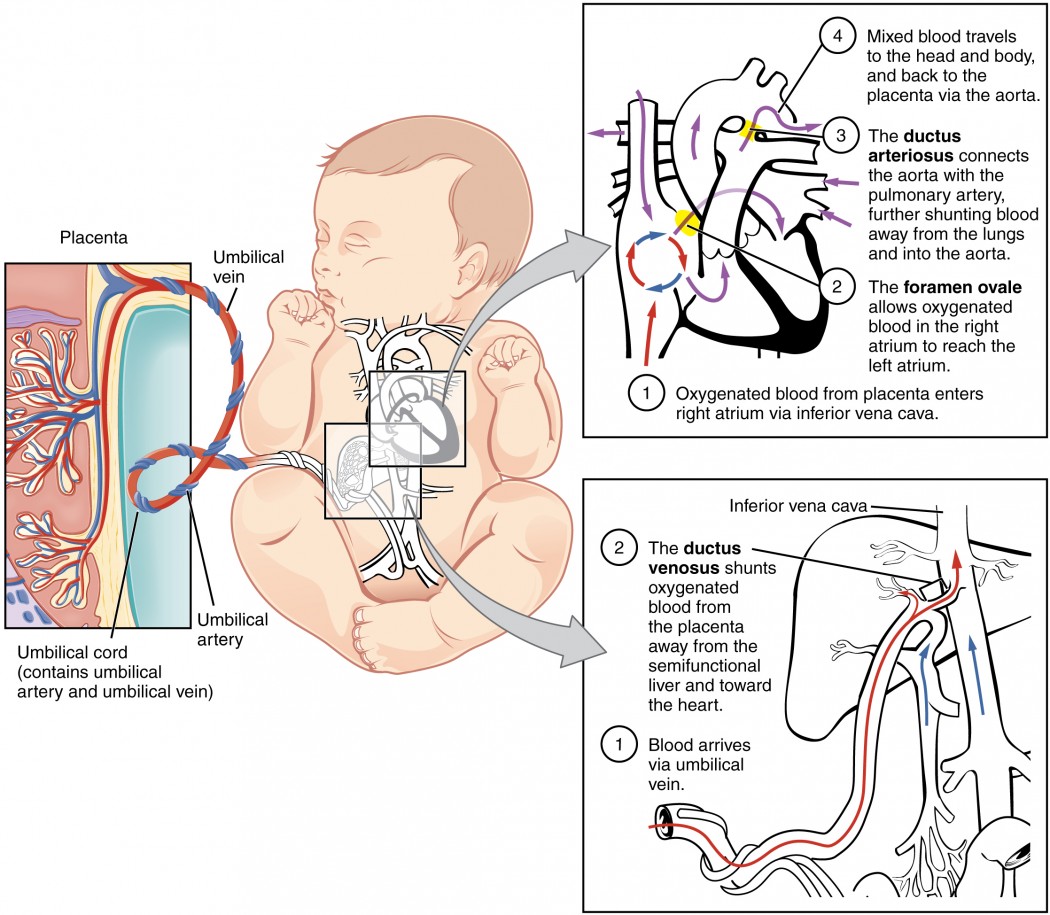
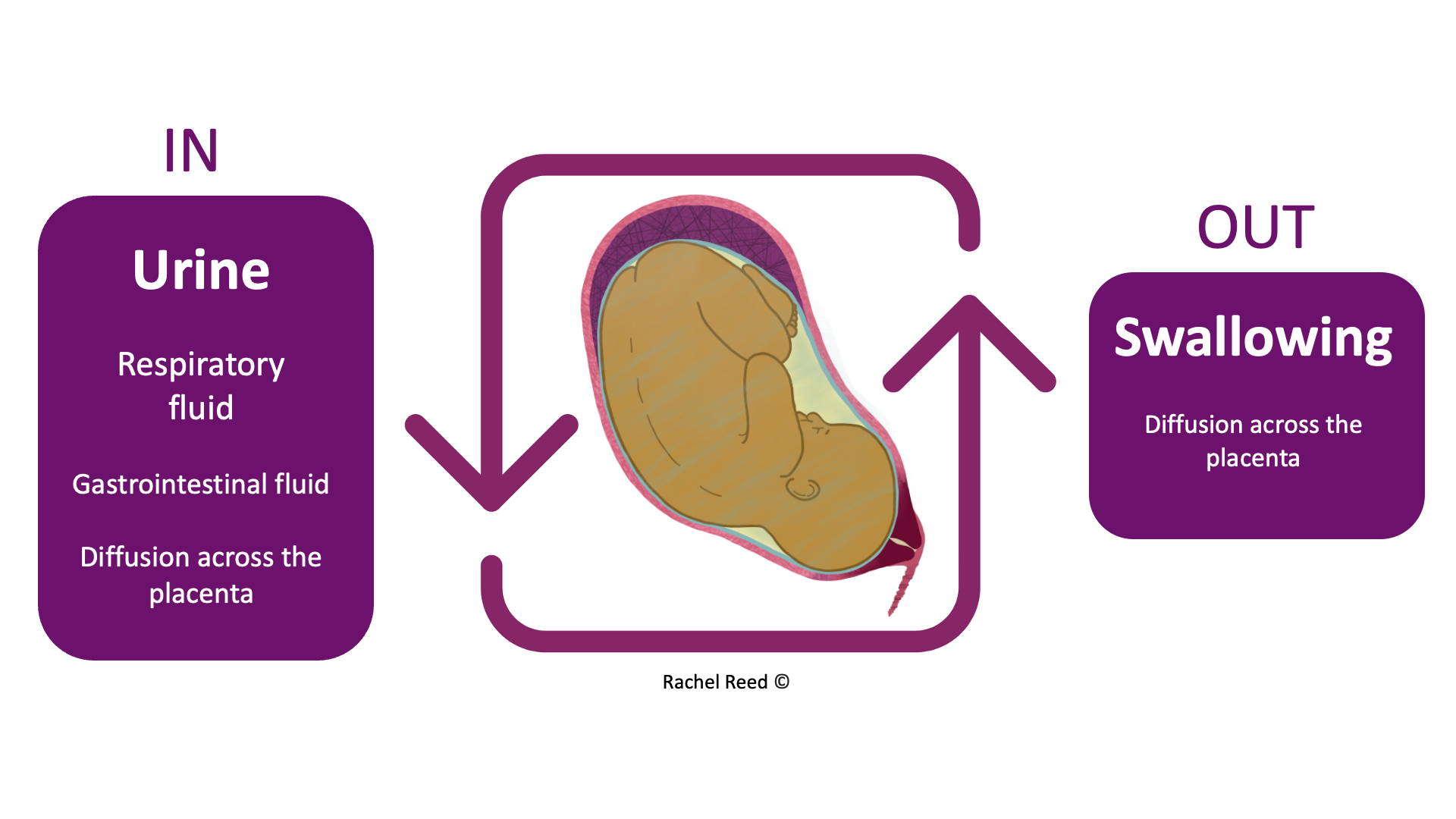
– Oxygen and carbon dioxide exchange in the womb occurs through the umbilical cord and placenta.
– After birth, babies initially rely on the umbilical cord and placenta for oxygen.
– Within about 10 seconds of delivery, babies take their first breath as they respond to the change in environment.
– By week 28 of pregnancy, the lungs of babies are fully developed enough that premature babies can breathe on their own.
– The lungs and circulatory system still need more time to mature.
– By week 37, the lungs have developed more fully and continue to grow and fine-tune until the child is at least 8 years old.
– The lungs begin producing surfactant at around month 6 of pregnancy, which allows them to inflate and deflate.
– Artificial surfactant can be used for babies born extremely preterm, along with breathing assistance from a ventilator, CPAP machine, or small breathing tubes.
– Babies born before week 36 and most born before week 32 may also need breathing support.
– A healthy pregnancy, quitting smoking, following a nutritious diet, avoiding smoke after birth, and encouraging regular exercise can support a baby’s lung development.
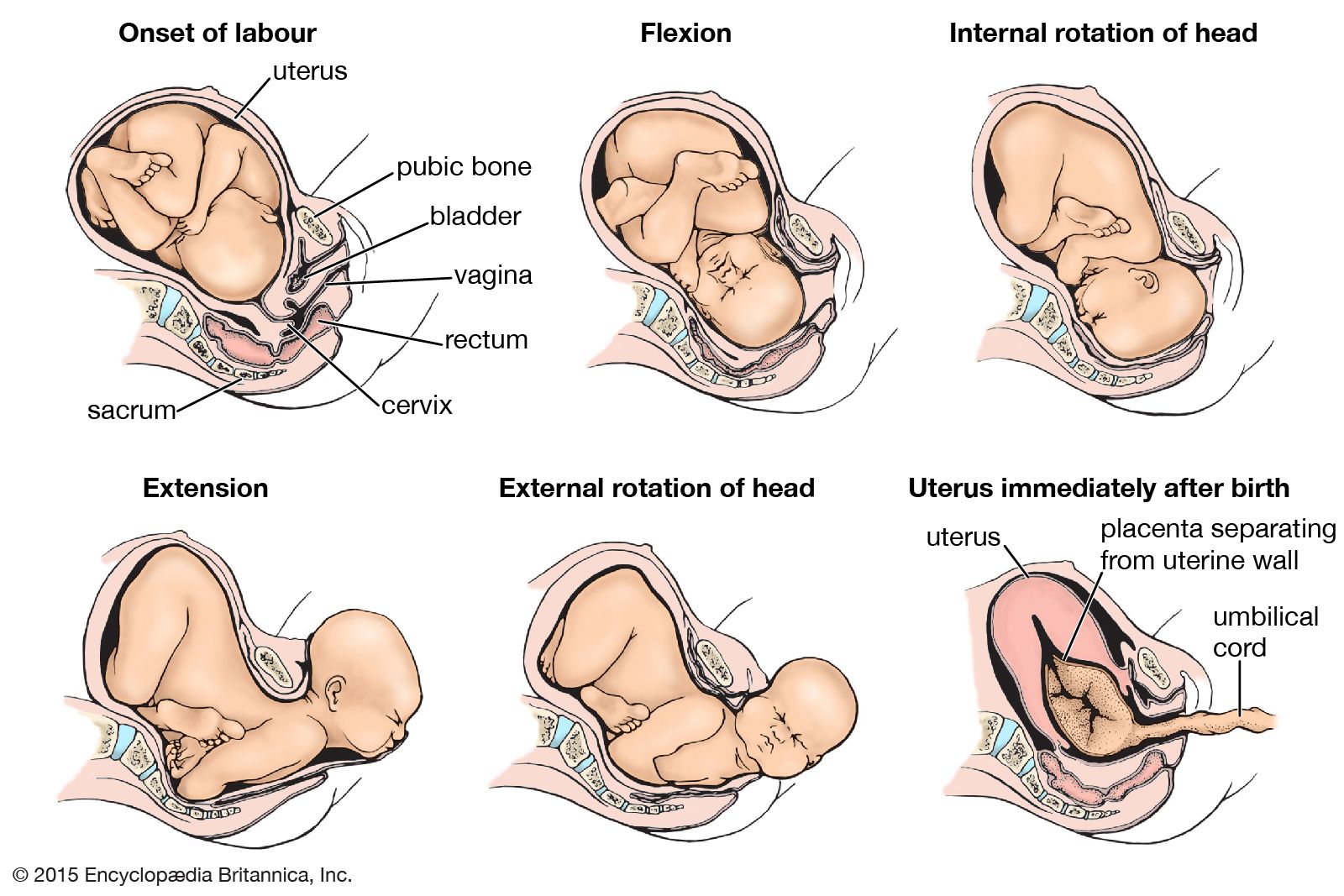
– Contractions during delivery squeeze the baby and force amniotic fluid out of the lungs, making it easier for them to breathe.
– As long as the baby is attached to the mother through the placenta and umbilical cord, it is not necessary for them to breathe.
– The baby will take their first breath a few seconds after delivery, without the support of the mother.
– The respiratory system is still growing after birth.
– Alveoli, small air sacs in the lungs, allow the body to transfer oxygen.
– Most newborns have between 20 and 50 million alveoli when born, which can increase to 300 million by the age of eight.
– The ribs surrounding the critical organs will get tougher as the baby develops, making the lungs more secure.
– Newborns may accidentally ingest meconium (first bowel movement) during birth, which can contaminate the lungs if not eliminated promptly.