Unlocking the Secrets of Persistent Occipitotransverse Position: A Comprehensive Guide
– Persistent occipitotransverse position
– Malpresentations and malpositions in obstetrics
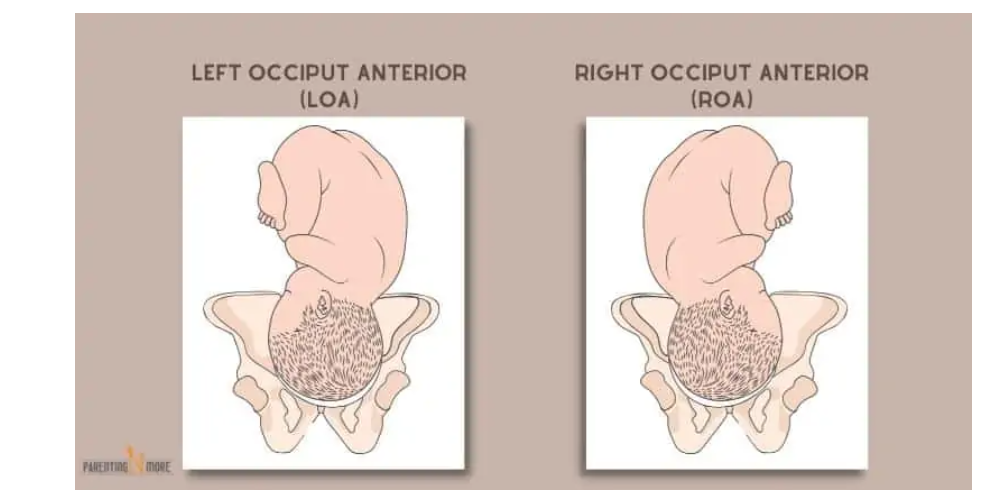
– Vertex presentation
– Left occipito-anterior position
– Right occipito-anterior position
– Defects in the powers
– Pendulous abdomen
– Defects in the passages
– Contracted pelvis
– Uterine anomalies
– Defects in the passenger
– Preterm fetus
– Multiple pregnancy
– Signs suggesting malpresentations
– Nonengagement of the presenting part
– Premature rupture of membranes
– Delay in descent of presenting part
– Complications of malpresentations
– Cord presentation and prolapse
– Prolonged labor
– Obstructed labor
– Instrumental and operative delivery
– Trauma to genital tract
– Postpartum hemorrhage
– Puerperal infection
– Perinatal mortality
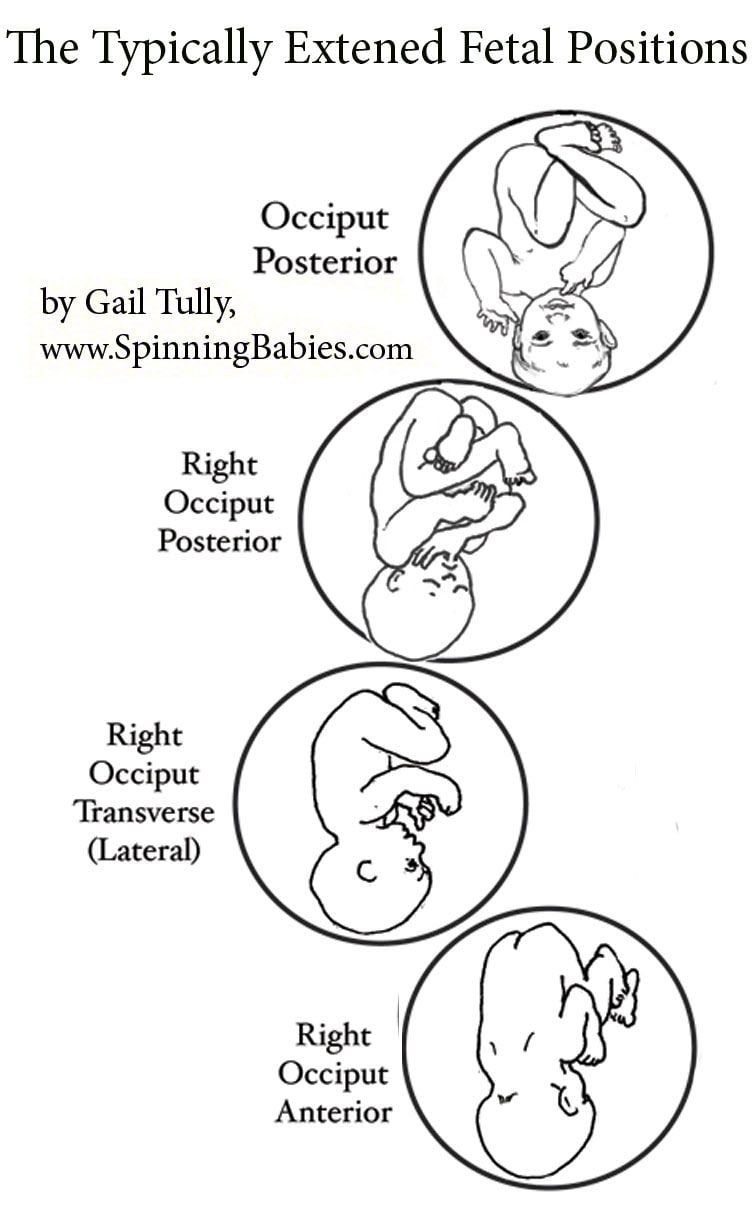
– Occipito-posterior position
– Right occipito-posterior
– Left occipito-posterior
– Shape of the pelvis
– Anthropoid pelvis
– Android pelvis
– Maternal kyphosis
– Anterior insertion of placenta
– Placenta previa
– Diagnosis of occipito-posterior position
– Ultrasonography
– Lateral view x-ray
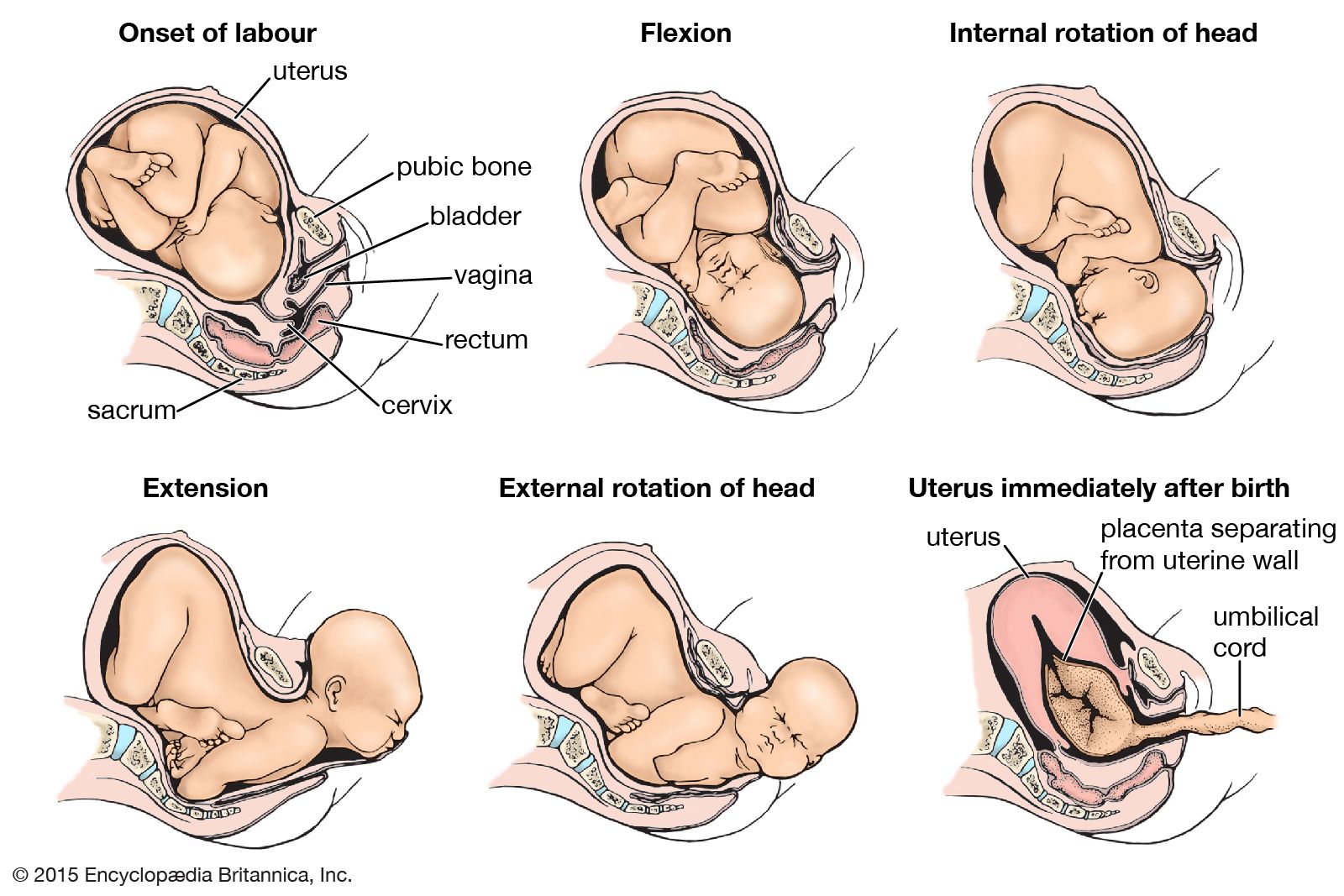
– Mechanism of labor
– Biparietal diameter
– Occipito-frontal diameter
– Deflexion of the occiput
– Normal mechanism of labor
– Abnormal mechanisms
– Deep transverse arrest
– Direct occipito-posterior
– Factors favoring long anterior rotation
– Well-flexed head
– Good uterine contractions
– Roomy pelvis
– Good pelvic floor
– Failure of long anterior rotation
– Uterine inertia
– Contracted pelvis
– Lax or rigid pelvic floor
– Management of labor
– Contracted pelvis
– Presentation or prolapse of cord
– Oxytocin
– Analgesia
– Premature rupture of membranes
– Second stage of labor
– Waiting for 60-90 minutes
– Observing mother and fetus
– Methods for management of persistent occipitotransverse position
– Internal rotation
– Direct occipito-posterior
– Deep transverse arrest
– Vacuum extraction
– Manual rotation
– Forceps
– Kielland’s forceps
– Barton’s forceps
– Scanzoni double application
– Caesarean section
– Craniotomy
– Preferred methods in modern obstetrics