Myoma of Uterus: Understanding Symptoms, Treatment, and Prevention
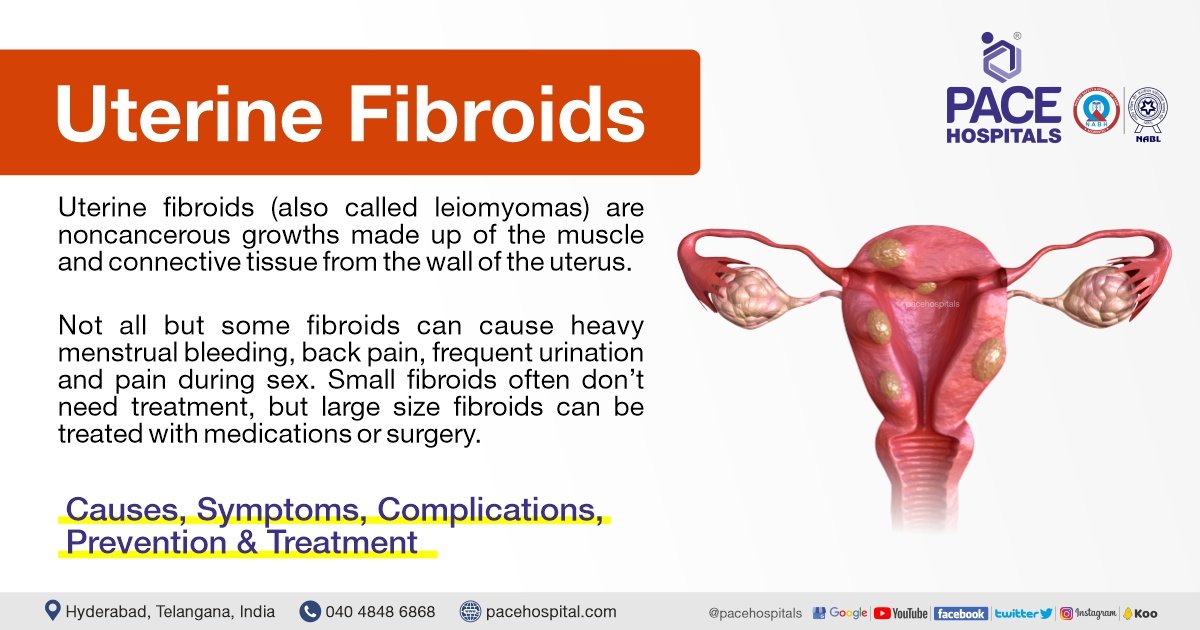
– A myoma, also known as a uterine fibroid or leiomyoma, is a common noncancerous tumor that grows in or around the uterus.
– Myomas can vary in size and may cause symptoms such as abdominal pain and heavy menstrual bleeding.
– Risk factors for myomas include a family history of myoma, obesity, and age.
– More than half of all people with a uterus will experience a myoma by age 50.
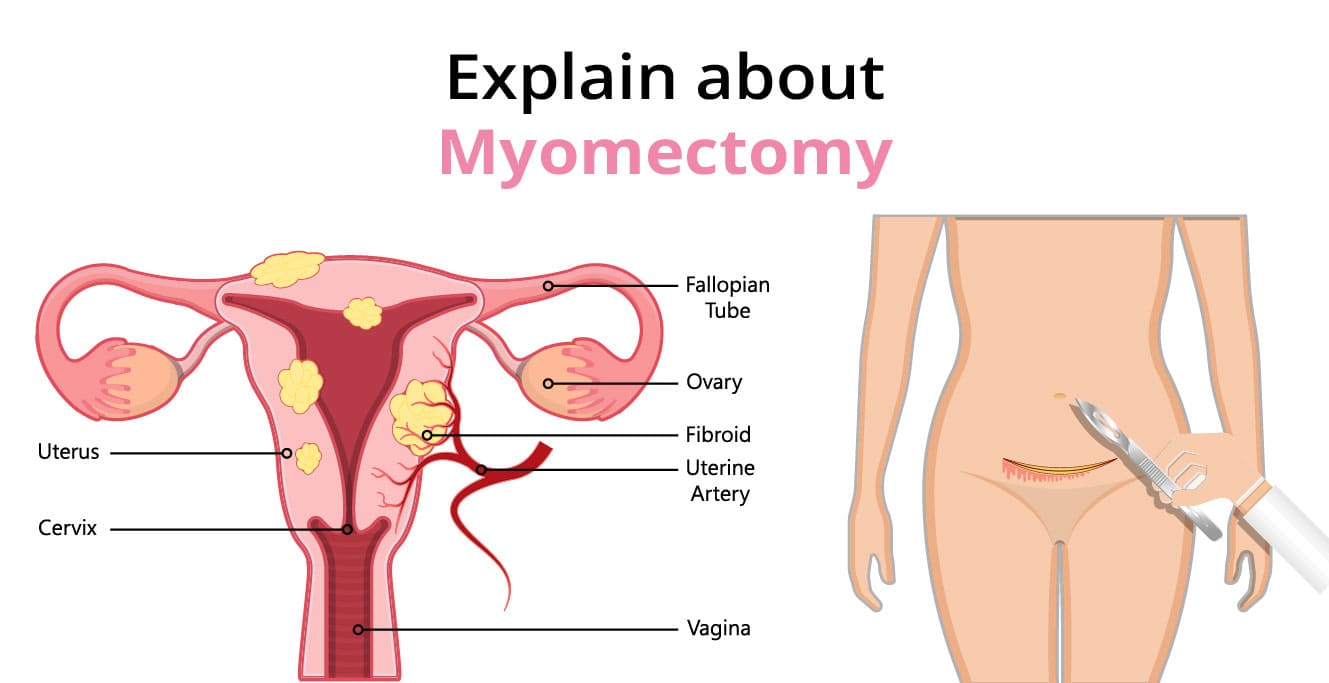
– Myomas can be categorized by location, size, and symptoms they may cause.
– Types of myomas include intramural myomas (located within the wall of the uterus), subserosal myomas (grow on the outside of the uterine wall), pedunculated myomas (develop a stalk or stem attaching them to the uterus), and submucosal myomas (found just under the lining of the uterus).
– A large myoma is considered to be 10 centimeters or more in diameter.
– Emergency room visits for myoma symptoms have increased from 2006 to 2017, including pelvic pain and heavy bleeding.
– Myomas are noncancerous growths that can cause various symptoms depending on their size and location.
– Symptoms of myomas include heavy and painful periods, bleeding between periods, pelvic pain, abdominal pressure, a feeling of fullness in the lower abdomen, constipation, diarrhea, frequent urination, pain during sex, lower back pain, trouble getting pregnant, fatigue, and weakness.
– Myomas are not life-threatening but can cause complications such as heavy blood loss or organ obstruction.
– Myomas are a top cause of hysterectomy surgeries.
– If a myoma bursts, immediate medical care is necessary.
– The exact cause of myomas is unknown but is likely associated with hormone activity, particularly high levels of estrogen and progesterone.
– Risk factors for myomas include a family history of the condition, obesity, high blood pressure, age, and certain dietary factors.
– Myomas are more common among Black people with a uterus.
– Diagnosis of myomas involves a series of steps, including medical history, physical examination, imaging tests such as ultrasound or MRI, and sometimes a biopsy.
– Treatment options for myomas include medication, noninvasive procedures, surgery, or a combination of therapies.
– Medications that may be used include over-the-counter pain medications, iron supplements, and birth control methods.
– Surgical options include laparoscopic myomectomy and uterine fibroid embolization (UFE).
– Lifestyle changes including dietary changes, exercise, stress management, and weight loss may improve symptoms and overall health.
– Complications of untreated myomas include fertility issues, pregnancy complications, and the need for cesarean delivery.
– It is important to discuss myomas with a healthcare provider before pregnancy for potential complications.
– Uterine fibroids, also known as myomas, are non-cancerous tumors that grow in the uterus.
– The most common symptom of myomas is vaginal bleeding.
– Other symptoms of myomas include heavy bleeding, anemia, fatigue, painful intercourse, pain, bleeding, or discharge from the vagina if myomas become infected, a feeling of pressure or lump in the abdomen, difficulties urinating, dribble at the end of urination, or urine retention if a myoma blocks the flow of urine.
– Myomas affect 20 percent of women in their childbearing years.
– The signs and symptoms of uterine fibroids include abnormal bleeding, pelvic masses, pelvic pain, infertility, and pregnancy complications.
– There are five types of uterine fibroids: intramural fibroids, subserosal fibroids, submucosal fibroids, pedunculated fibroids, and intracavitary fibroids.
– Between 70 and 80 percent of women develop a fibroid tumor by the time they reach age 50.
– Estrogen seems to activate the growth of uterine fibroids, and they shrink after menopause, but hormone therapy after menopause may cause their symptoms to continue.
– Factors associated with the development of uterine fibroids include race, age, early menstruation, caffeine and alcohol intake, genetics, obesity, high blood pressure, and diet.
– Nearly one-third of women with uterine fibroids seek treatment because of the severity of their symptoms.
– Treatment options for uterine fibroids include hormonal contraception, intrauterine devices, antifibrinolytic nonsteroidal agents, endometrial ablation, medications called gonadotropin-releasing hormone agonists, myomectomy, MRI-guided ultrasound surgery, and uterine fibroid embolization.
– Uterine fibroid embolization is a minimally invasive option that blocks the blood supply to fibroids, causing them to shrink and die.
– Myoma, leiomyoma, and uterine fibroids all refer to the same thing, a non-cancerous tumor of the uterus.
– The management of uterine fibroids, also known as myomas, requires further research to improve treatment outcomes.