– Pelvic inflammatory disease (PID) is an infection of a woman’s reproductive organs
– PID is often caused by STDs like chlamydia and gonorrhea
– Other non-sexually transmitted infections can also cause PID
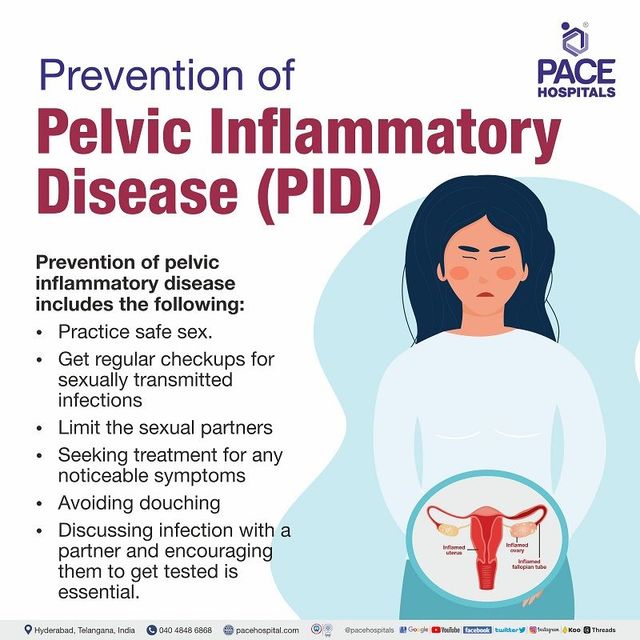
– Factors that increase the risk of PID include having an untreated STD, having multiple sex partners, having a partner with other sex partners, a history of PID, being sexually active and under the age of 25, douching, and using an intrauterine device for birth control
– To reduce the risk of getting PID, it is recommended to practice abstinence or have sex in a long-term mutually monogamous relationship and use condoms correctly
– There are no specific tests for PID, and diagnosis is based on medical history, physical examination, and other test results
– Symptoms of PID can include lower abdominal pain, fever, unusual discharge with a bad odor from the vagina, pain or bleeding during sex, burning sensation during urination, and bleeding between periods
– It is important to see a doctor if these symptoms occur, if there is a suspicion of an STD, or if there are any genital symptoms
– PID can be cured with early diagnosis and treatment, but damage to the reproductive system cannot be reversed
– It is crucial to complete the full course of antibiotics and inform recent sex partners for testing and treatment
– PID can be transmitted to a sexual partner, so it is important for both partners to receive treatment
– If PID is not treated early, it can lead to complications such as scar tissue formation in the fallopian tubes, which can cause blockages
– Other complications include ectopic pregnancy (pregnancy outside the womb), infertility, and long-term pelvic or abdominal pain
– Ways to reduce the risk of getting PID include abstaining from vaginal, anal, or oral sex, being in a long-term mutually monogamous relationship with a partner who has tested negative for STDs, and using latex condoms correctly
– Diagnosis of PID is usually based on medical history, physical examination, and other test results
– It is important to see a doctor if any symptoms of PID occur or if there is a suspicion of STD exposure
– PID can be cured if diagnosed early, but treatment cannot reverse damage already done to the reproductive system
– Partners should also be informed to get tested and treated for STDs
– Having had PID before increases the chances of getting it again
– Early treatment of PID can prevent complications such as the formation of scar tissue outside and inside the fallopian tubes, which can lead to tubal blockage
Continue Reading