Exploring the Intricate Cavity of the Uterus: Unveiling Mysteries
List of pertinent information about the cavity of the uterus (no duplications):
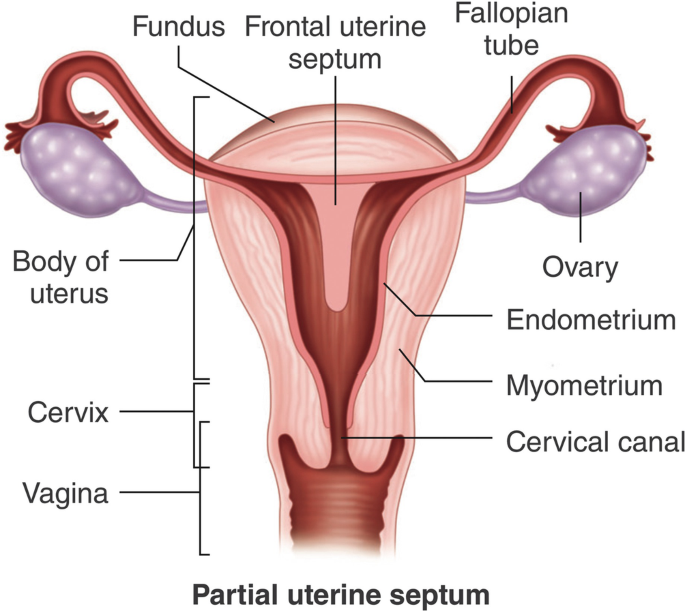
– The uterine cavity is the inside portion of the uterus.
– It is triangular in shape and formed by the internal surface of the body of the uterus.
– The base of the cavity is located between the openings of the fallopian tubes.
– The apex is the internal opening of the uterus that connects to the cervix.
– The part of the uterine cavity that enters the openings of the fallopian tubes is a narrow, flattened area.
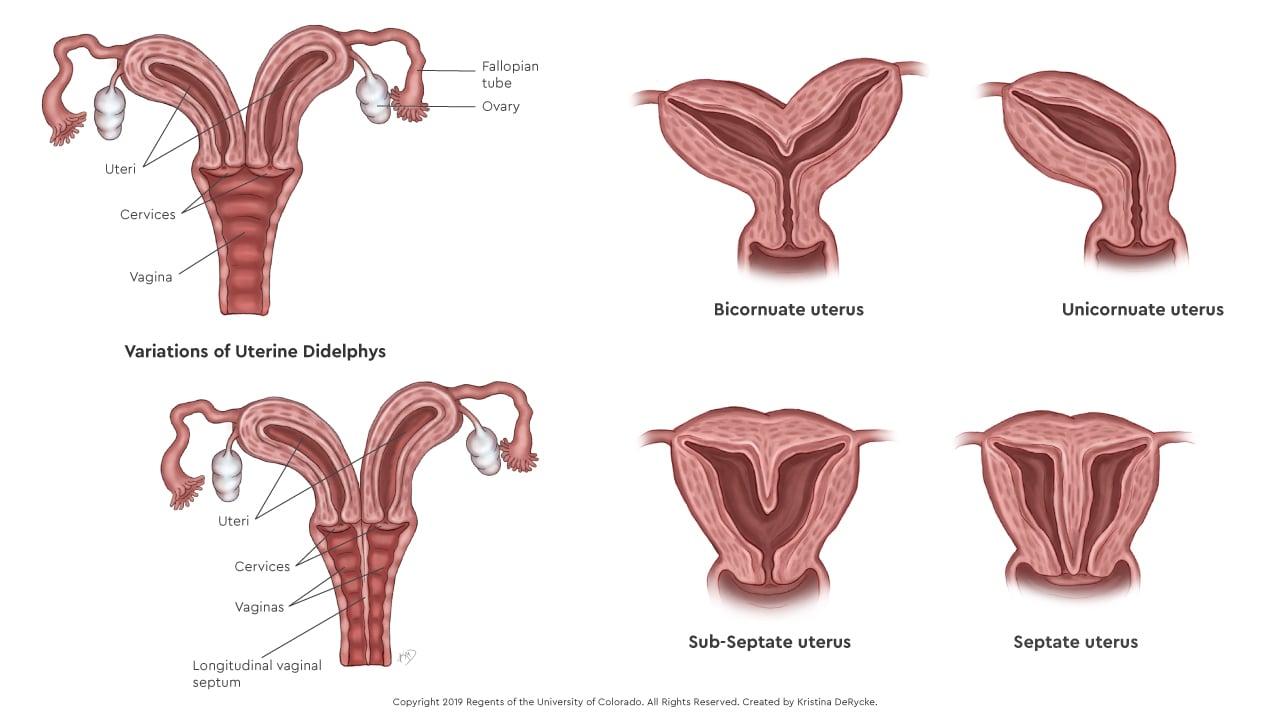
– Abnormalities of the womb or congenital uterine abnormalities refer to women who have a womb that is different in shape or size from the norm.
– These abnormalities can be discovered during an ultrasound scan or if a woman experiences miscarriage, bleeding, or difficulties conceiving.
– Women with womb abnormalities may have an increased risk of miscarriage, preterm birth, or fertility problems depending on the shape of the womb.
– Women with bicornuate wombs have a slightly higher risk of miscarriage and preterm birth.
– Women with a unicornate womb have half the size of a normal womb and an increased risk of ectopic pregnancy, late miscarriage, or preterm birth.
– Women with a didelphic womb, which is split in two, may have a small increased risk of preterm birth.
– Women with a septate/subseptate womb may have an increased risk of miscarriage, preterm birth, or fertility problems.
– Septate wombs may cause difficulties with conception.
– Septate wombs have an increased risk of early miscarriage and preterm birth.
– Babies in later pregnancy with septate wombs may not be in a head-down position, leading to a higher likelihood of needing a C-section.
– Many women with congenital uterine abnormalities, like a septate uterus, are not aware of their condition.
– Surgery to resect the septum before pregnancy is common for women with a septate uterus, but it was not recommended by the consultant in this case.
– Despite having a complete septate uterus, the woman in the case was able to carry her baby to term but had an elective C-section because the baby was breech.
– An arcuate womb has a dip at the top but resembles a normal womb.
– Having an arcuate womb does not increase the risk of preterm birth or early miscarriage.
– An arcuate womb may increase the risk of late miscarriage.
– Babies in later pregnancy with an arcuate womb may not be in a head-down position, increasing the likelihood of needing a C-section.