Contraction Stress Testing: A Comprehensive Guide for Expectant Mothers
– A contraction stress test (CST) is a test for pregnant people to check their baby for signs of stress during uterine contractions.
– The test involves the administration of a hormone that causes the uterus to contract, similar to labor contractions.
– The purpose of the test is to see if the baby can tolerate the temporary decrease in blood and oxygen supply that occurs during labor contractions.
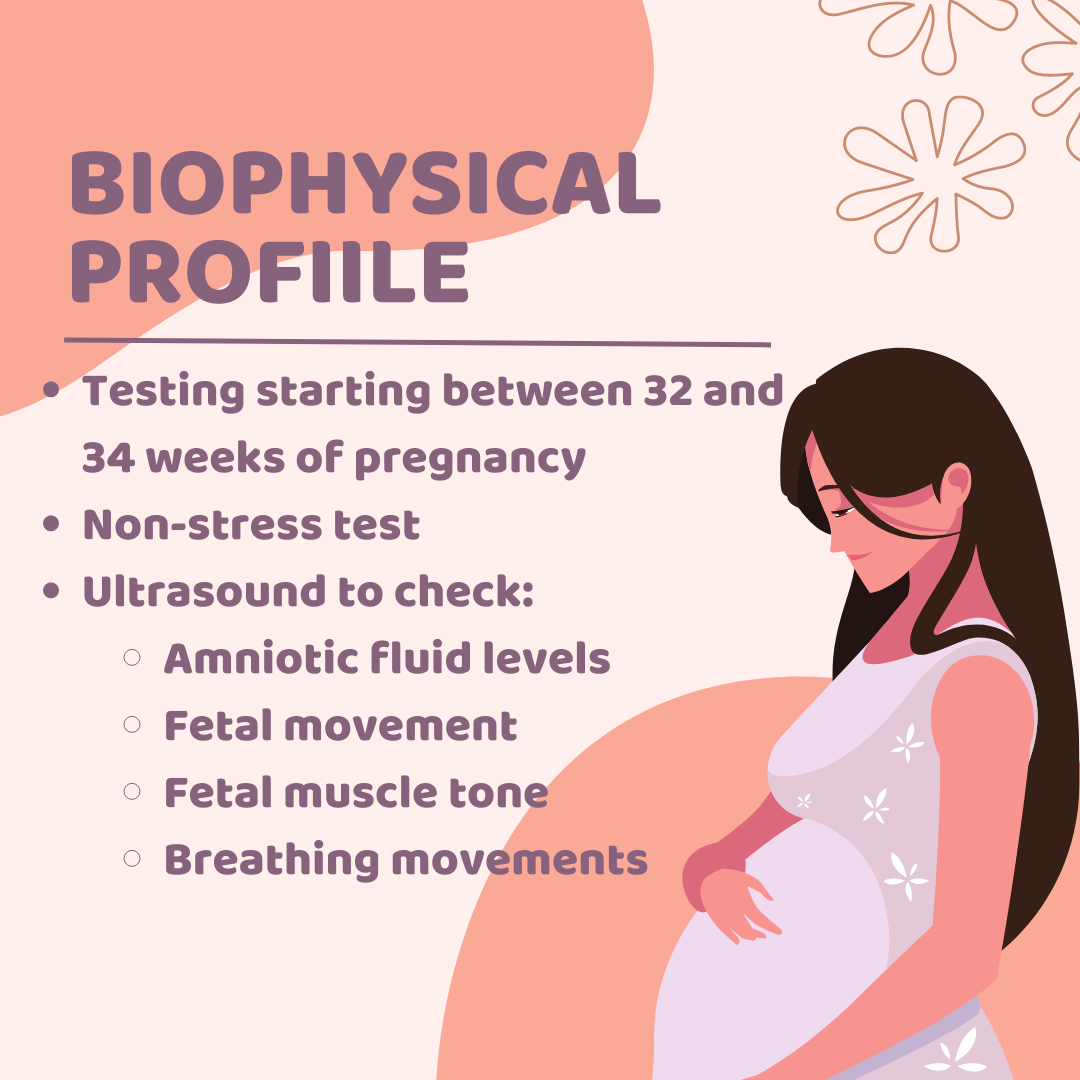
– A CST is usually performed if a nonstress test or biophysical profile shows atypical results.
– Nonstress tests check the baby’s heart rate and oxygen supply and are typically done around 28 weeks of pregnancy.
– Biophysical profiles combine a nonstress test with ultrasound imaging to assess the baby’s heart rate, breathing, muscles, and movements.
– A contraction stress test is performed when a person is 34 weeks or more pregnant.
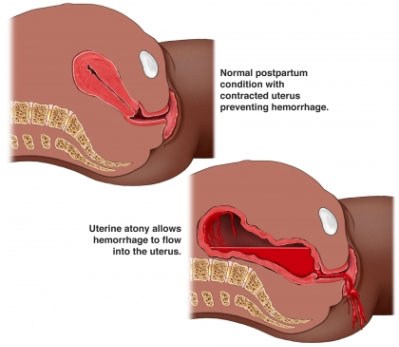
– A contraction stress test measures the fetal heart rate after the mother’s uterus is stimulated to contract.
– The test is done to ensure that the fetus can handle contractions during labor and receive enough oxygen from the placenta.
– It is recommended when a nonstress test or biophysical profile indicates a problem.
– The test can determine if the baby’s heart rate remains stable during contractions.
– It may be scheduled if the doctor is concerned about how the baby will respond to contractions or to observe the fetal heart rate response to stimulation.
– The test can induce labor.
– The uterus is stimulated with pitocin, a synthetic form of oxytocin, either through injections or by squeezing the mother’s nipples.
– The results of a contraction stress test are available right away.