New Research Revealed: The Shocking Truth About Abruption
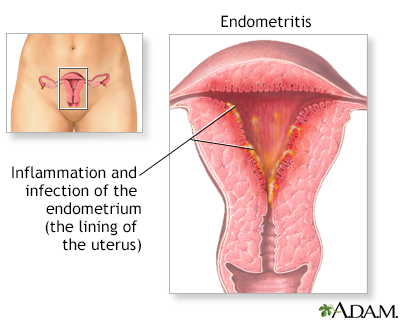
– Placental abruption is when a part or all of the placenta separates from the uterus prematurely, causing vaginal bleeding.
– There are two main types of placental abruption: revealed and concealed. Revealed abruption results in visible vaginal bleeding, while concealed abruption involves bleeding that remains within the uterus and may not be visible.
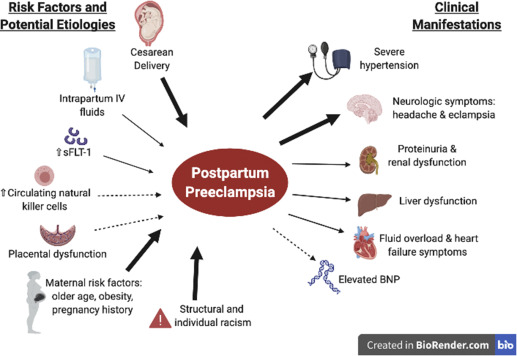
– Major risk factors for placental abruption include previous placental abruption, pre-eclampsia, abnormal lie of the baby, abdominal trauma, smoking or drug use, bleeding in the first trimester, and underlying thrombophilias.
– Clinical features of placental abruption include painful vaginal bleeding, woody and painful uterus on palpation, and the need for systematic assessment and resuscitation.
– General examination involves assessing pallor, distress, peripheral circulation, abdominal tenderness, the feel of the uterus, and the lie and presentation of the fetus/fetuses. The article provides guidance on how to assess bleeding during pregnancy and discusses differential diagnoses for antenatal hemorrhage. It suggests using a cardiotocograph (CTG) at 26 weeks gestation or above to check fetal wellbeing. It advises checking hand-held pregnancy notes for scan reports and looking for signs of placenta praevia. The article also recommends assessing the bleeding externally by looking at pads, avoiding speculum examination until placenta praevia is excluded, and taking triple genital swabs to exclude infection. It warns against performing a digital vaginal examination with known placenta praevia as it could cause massive bleeding. The article mentions placental abruption, placenta praevia, marginal placental bleed, vasa praevia, uterine rupture, and local genital causes as differential diagnoses for antenatal hemorrhage.
– Placental abruption is a common cause of antepartum hemorrhage.
– Investigations that should be performed include hematology (full blood count, Kleihauer test, group and save, cross-match), biochemistry (urea and electrolytes, liver function tests), and fetal wellbeing assessment (cardiotocograph).
– Ultrasound scan should be performed to assess placental abruption, but ultrasound should not be used to exclude abruption.
– Management of placental abruption depends on the health of the fetus: emergency delivery is indicated in the presence of maternal and/or fetal compromise, induction of labor is recommended for hemorrhage at term without compromise, and conservative management is an option for some partial or marginal abruptions without compromise.
– Anti-D should be given within 72 hours of bleeding onset if the woman is rhesus D negative.
– Placental abruption complicates approximately 1% of pregnancies and increases the risk of maternal, fetal, and neonatal morbidity and mortality.
– Risk factors for placental abruption include smoking, alcohol or cocaine use during pregnancy, advanced maternal age, history of maternal hypertension, and preeclampsia.
– Previous placental abruption and multiple gestational pregnancies also increase the risk.
– Trauma from a motor vehicle accident, fall, or blow to the abdomen can cause placental abruption.
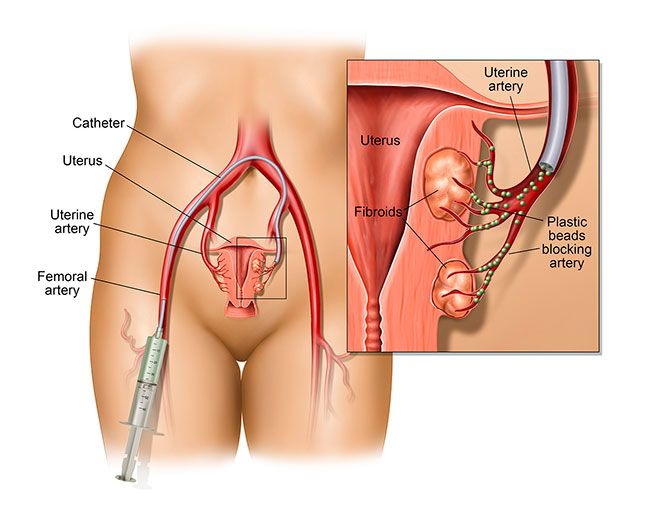
– Radiologic imaging, such as ultrasonography, may assist in diagnosing placental abruption.
– Ultrasonography is usually the preferred study due to its benefits of avoiding ionizing radiation, dynamic nature, and availability.
– In severe trauma cases, CT scanning may be required to evaluate for abdominopelvic injuries.
– American College of Radiology guidelines recommend ultrasound FAST scan as a limited bedside adjunct for triage in a pregnant patient with major blunt trauma. The article discusses the use of imaging techniques for diagnosing major blunt trauma in pregnant patients. The American College of Radiology (ACR) states that there are two options for these procedures, but only one should be used to gather clinical information. No other facts, stats, or figures are mentioned in the article.