– Aberrations in uterine bleeding are now referred to as abnormal uterine bleeding (AUB) and dysfunctional uterine bleeding (DUB)
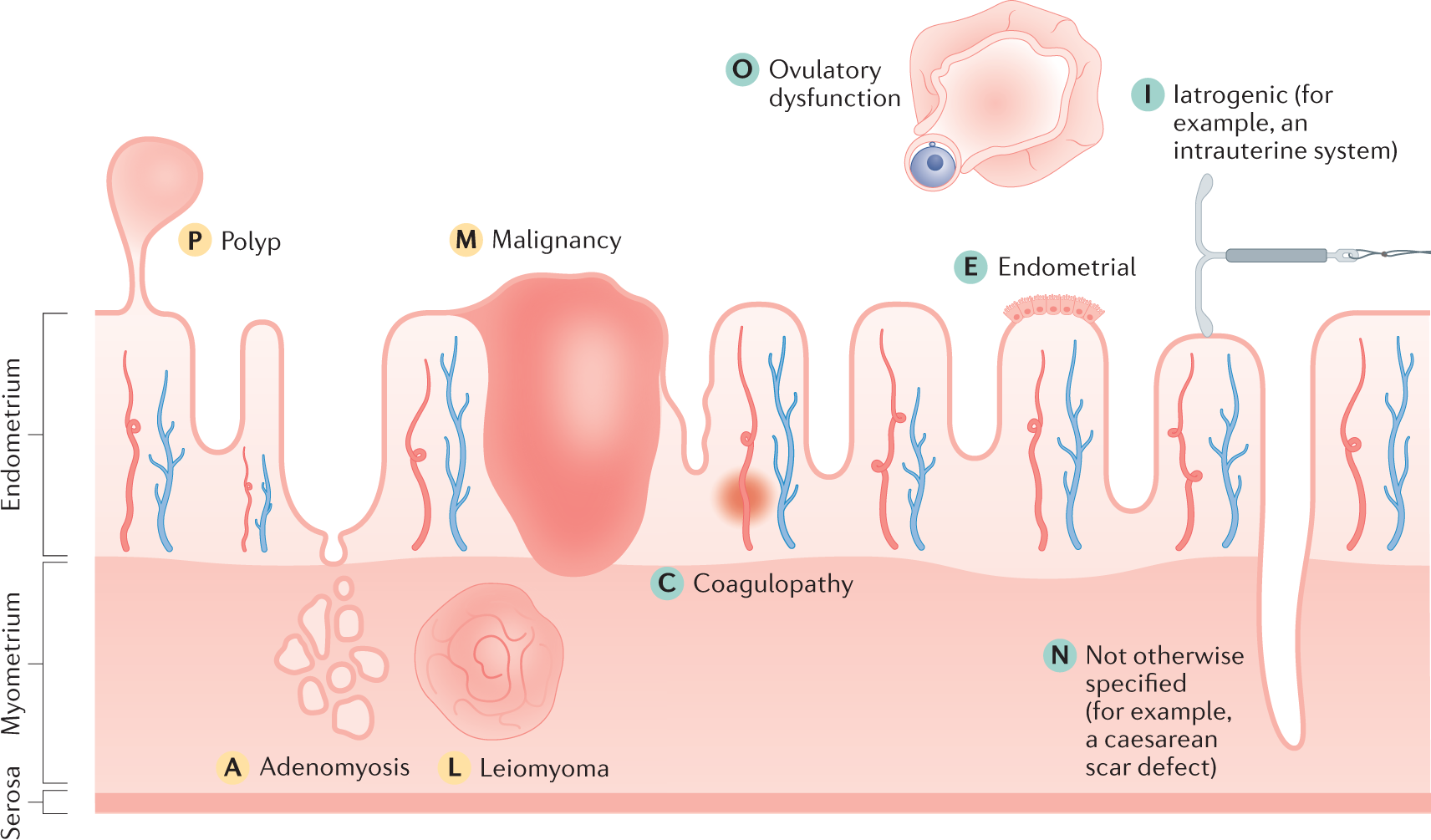
– In 2011, the Fédération International de Gynécologie et d’Obstétrique (FIGO) defined causes of AUB using the acronym PALM-COEIN to standardize etiologies
– AUB is defined as a change in volume, regularity, or timing that has been present for 6 months or longer
– AUB affects 14-25% of women of reproductive age and is a major cause of loss of work and productivity
– Symptoms of AUB can include irregular or excessive bleeding, with excessive volume defined as an amount greater than 80 mL
– Symptoms of endometrial polyps include intermenstrual bleeding and may be asymptomatic in one-third of cases
– Symptoms of adenomyosis include heavy menses, dysmenorrhea, and midline dyspareunia
– Symptoms of leiomyomata (fibroids) depend on their size and location, with submucosal fibroids resulting in heavy unpredictable bleeding and intramural fibroids resulting in heavy but predictable bleeding
– Endometrial cancer is the most common cause of AUB-M, with postmenopausal bleeding being a common symptom
– In patients with coagulopathies, AUB typically presents in adolescence with the most common patterns being heavy menses and heavy irregular menses
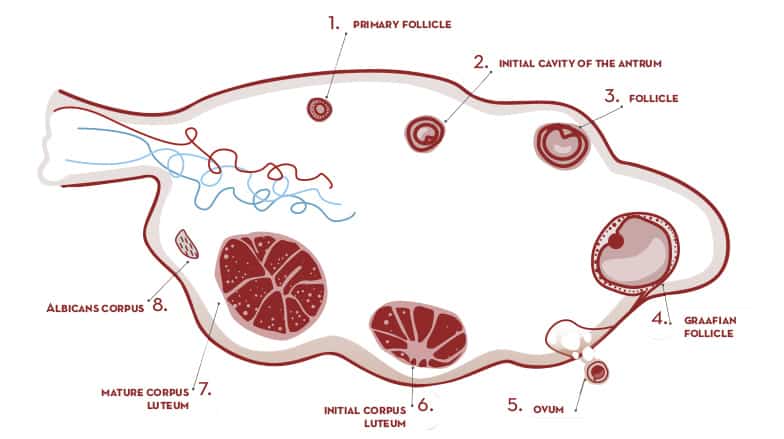
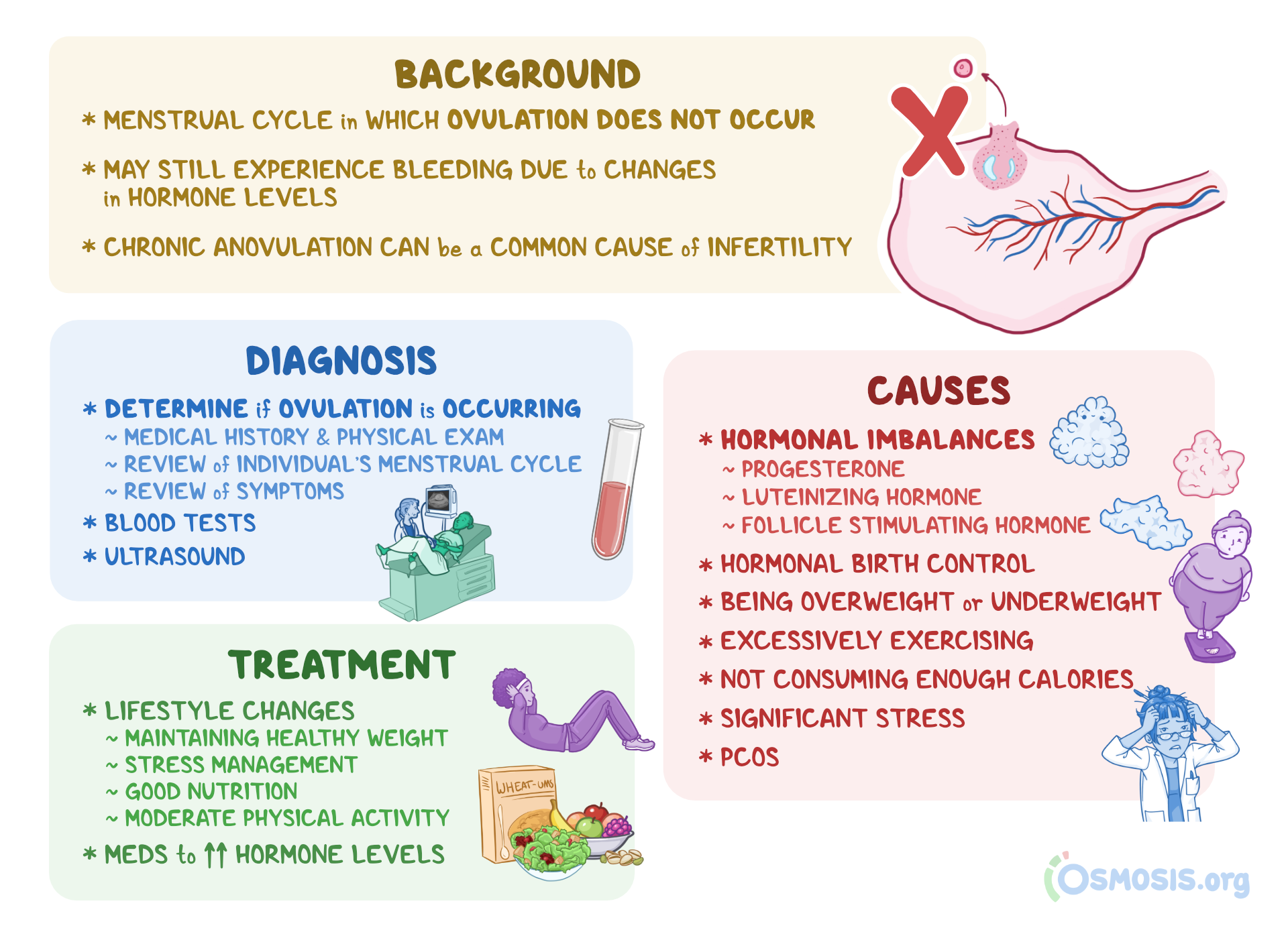
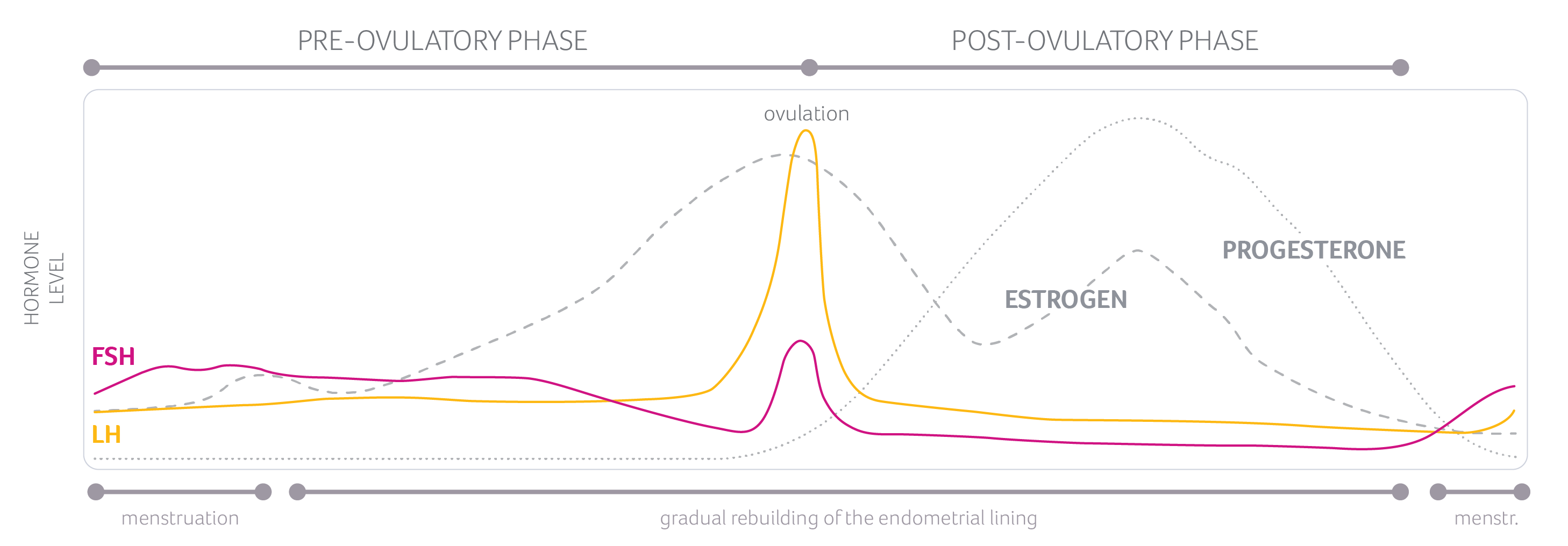
The article discusses ovulatory dysfunctional uterine bleeding (AUB), which is a common type of abnormal uterine bleeding. There are different subtypes of AUB, including ovulatory dysfunction (AUB-O), primary endometrial dysfunction (AUB-E), iatrogenic causes (AUB-I), and etiologies not otherwise classified (AUB-N). A complete history and physical examination should be conducted to establish a differential diagnosis and targeted laboratory and imaging studies may be necessary. Laboratory tests may include hormone levels such as human chorionic gonadotropin (hCG), thyroid-stimulating hormone (TSH), prolactin, follicle-stimulating hormone (FSH), estradiol (E2), and luteinizing hormone (LH). Women with signs of androgen excess should have tests for testosterone, dehydroepiandrostenedione sulfate (DHEAS), and 17-hydroxyprogesterone (17OHP). Screening for certain conditions, such as Cushing disease, may also be necessary. Prothrombin time (PT), activated partial thromboplastin time (aPTT), fibrinogen, von Willebrand panel, platelet function, and coagulation factor levels should be tested for patients with AUB-C, especially if they have heavy bleeding and a history of easy bruising or bleeding from dental extraction, surgery, or the nose. Women should also have an up-to-date Pap test and human papillomavirus (HPV) testing. Imaging studies may be necessary for women with an abnormal uterus or specific bleeding patterns. This article provides information on uterine evaluation and treatment options for ovulatory dysfunctional uterine bleeding (AUB-O). The optimal imaging study depends on the specific disease process. Hysteroscopy is the best diagnostic tool for detecting polyps, while a saline infusion sonogram (SIS) is the best screening test for fibroids. Adenomyosis is best evaluated with a magnetic resonance imaging (MRI) scan, but a standard transvaginal ultrasound (TVUS) can also be used. Endometrial testing is recommended for women aged 45 and older to exclude endometrial cancer. In premenopausal patients, there are no specific ultrasound findings or endometrial thickness measurement to exclude cancer. In postmenopausal women not taking hormones, an endometrial thickness of 4 mm or less has a 94.8% sensitivity for excluding cancer. Endometrial evaluation should also be considered in women under 45 with certain conditions such as obesity, diabetes, polycystic ovary syndrome (PCOS), failed previous therapy, and prolonged estrogen exposure. Women with Lynch syndrome should undergo annual screening with endometrial biopsy and TVUS starting at age 25. Women on tamoxifen with bleeding and those with estrogen-producing ovarian tumors also require endometrial evaluation. Treatment depends on the cause of the ovulatory dysfunctional bleeding and can include hysteroscopy for polyp removal, constant progestin exposure, elimination of systemic estrogen, or surgical intervention for symptomatic adenomyosis. This article discusses the treatment options for different types of abnormal uterine bleeding. For ovulatory dysfunctional uterine bleeding, continuous progestin therapy can provide pain relief. If progestin therapy does not work, estrogen deprivation can be induced with a gonadotropin-releasing hormone agonist or an oral GnRH antagonist. Vaginal symptoms may benefit from vaginal moisturizers or low-dose vaginal estrogen. Hysterectomy is recommended for those who do not desire future pregnancy, while uterine artery embolization is an option for those who do not want a hysterectomy. Endometrial ablation is not effective for treating adenomyosis. The treatment of fibroids depends on size, location, and symptoms. Hysteroscopic myomectomy is preferred for those who desire childbearing, while hysterectomy is an option for those with complete families. Estrogen deprivation can be used to induce amenorrhea until surgery in anemic patients. Intramural fibroids may benefit from suppressing endometrial growth with progestin therapy, and surgical intervention options depend on the desire for childbearing. The management of endometrial cancer is not discussed in this article. Coagulation disorders causing abnormal bleeding can be treated according to the underlying cause, with options including tranexamic acid and desmopressin. In severe cases, von Willebrand factor concentrates or recombinant activated factor VII may be considered. Medical induction of amenorrhea is generally the preferred option for treating coagulation disorders. Summary: This article discusses the treatment options for ovulatory dysfunctional uterine bleeding. The most common bleeding disorder associated with ovulatory dysfunction is chronic anovulation due to polycystic ovary syndrome (PCOS). PCOS results in prolonged unopposed estrogen with continuous endometrial proliferation and unpredictable structural breakdown. Treatment for this condition requires chronic therapy, usually with continuous or sequential progestin exposure. Hormonal therapies such as combined oral contraceptives (COCs), progestin-secreting intrauterine devices (IUS), implants, and various progestin medications can be used. Acute treatment for heavy bleeding depends on the severity of the bleeding and the patient’s stability, and may involve the use of intravenous conjugated equine estrogens, monophasic COCs, or tranexamic acid. Common side effects of hormonal therapy include nausea, vomiting, and breast tenderness. There is a significant risk of venous thrombotic events with estrogen treatment, so non-estrogen options should be considered for women with thrombophilia or other risk factors. Tranexamic acid has an FDA warning against concomitant use with estrogen products, but studies are lacking on this interaction. The article discusses different types of ovulatory dysfunctional uterine bleeding (AUB) and their respective treatment options. AUB-E is primarily a diagnosis of exclusion and is characterized by heavy menses in ovulatory women. Treatment options for AUB-E include progestin-secreting intrauterine systems (IUS), combined oral contraceptives (COC), tranexamic acid, and nonsteroidal anti-inflammatory drugs (NSAIDs). Some authors also include chronic endometritis in this category. Endometritis can be diagnosed by the presence of plasma cells in an endometrial biopsy during the follicular phase, and empirical treatment with antibiotics such as doxycycline or a combination of a quinolone and metronidazole can be effective. For women who have completed their families, endometrial ablation or hysterectomy may be considered. AUB-I refers to iatrogenic causes of AUB, such as medications that affect the integrity of the endometrium like continuous progestins and induction of chronic endometritis with intrauterine devices. Treating AUB-I may involve short courses of vaginal estrogen or addressing inflammation related to intrauterine device use. AUB-N refers to non-specific causes of AUB, with one possibility being delayed postpartum hemorrhage due to subinvolution of the placental site. This condition can be treated with intravenous conjugated equine estrogen therapy, while dilation and curettage should be avoided.
Continue Reading