– A hydatidiform mole, or molar pregnancy, is a rare condition affecting approximately 1 in 1,200 pregnancies.
– It is typically detected in early pregnancy and can be identified through ultrasound or examination of tissue after a miscarriage.
– In a molar pregnancy, there is abnormal and rapid growth of part or all of the placenta, resulting in a larger than normal size and the presence of fluid-filled cysts.
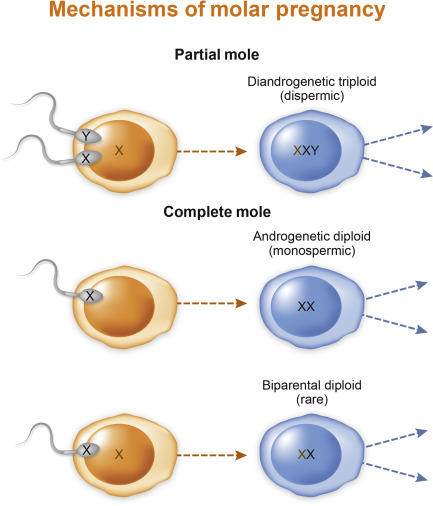
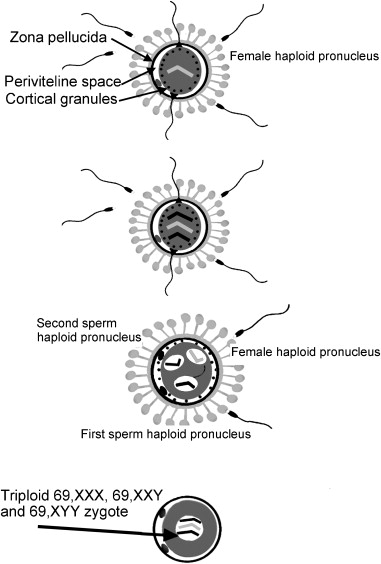
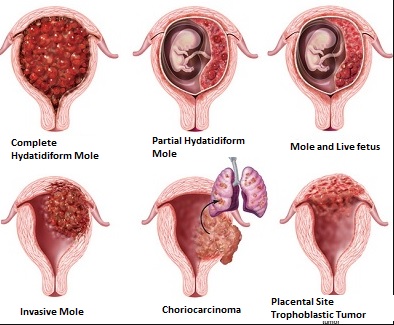
– Two types of molar pregnancy include complete molar pregnancy, in which a fetus does not develop, and partial molar pregnancy, in which a fetus develops but is abnormal and cannot survive beyond three months.
– Despite the abnormal pregnancy, women may still experience typical symptoms such as morning sickness or sore breasts due to the production of the pregnancy hormone hCG by the placenta.
– In some cases, the placenta can become malignant and develop into choriocarcinoma, a rare form of cancer that can spread to organs like the lungs, liver, and brain. Choriocarcinoma responds well to chemotherapy.
– Risk factors for molar pregnancy include age (under 18 or over 35), Asian or Mexican background, a diet low in carotene, and a history of previous molar pregnancy or other gestational trophoblastic tumor.
– Registries like the Gestational Trophoblastic Disease (GTD) Registry at the Royal Women’s Hospital are established to monitor and provide follow-up care for women who have had a molar pregnancy.
– Regular monitoring of hCG levels is necessary to detect any remaining molar cells that could grow and potentially spread to other organs. Testing involves urine and blood collection, and treatment may be required if hCG levels do not decrease.
– It is important to avoid getting pregnant again until discharged from the registry to prevent confusion between a new pregnancy and persistent trophoblastic disease. After discharge, attempting a new pregnancy is safe after having at least one normal period and using contraception during this time.
– Emotional healing after a molar pregnancy can take a longer time than physical healing from treatment, and seeking support from family, friends, and the GTD Registry team is recommended.
Continue Reading