– The study will be conducted in hospitals in Australia that have 2,000 or more deliveries per year.
– The intervention will be performed by experienced obstetricians or midwives.
– The inclusion criteria for the study include being at least 18 years old, having a singleton pregnancy, being at least 37 weeks gestation, planning a vaginal birth, having a cephalic presentation, and having confirmed occiput transverse position.
– The exclusion criteria include clinical suspicion of cephalopelvic disproportion, previous caesarean section, brow or face presentation, pathologic CTG, fetal scalp abnormalities, chorioamnionitis, intrapartum hemorrhage, maternal diabetes, suspected fetal bleeding disorder, and major fetal abnormalities.
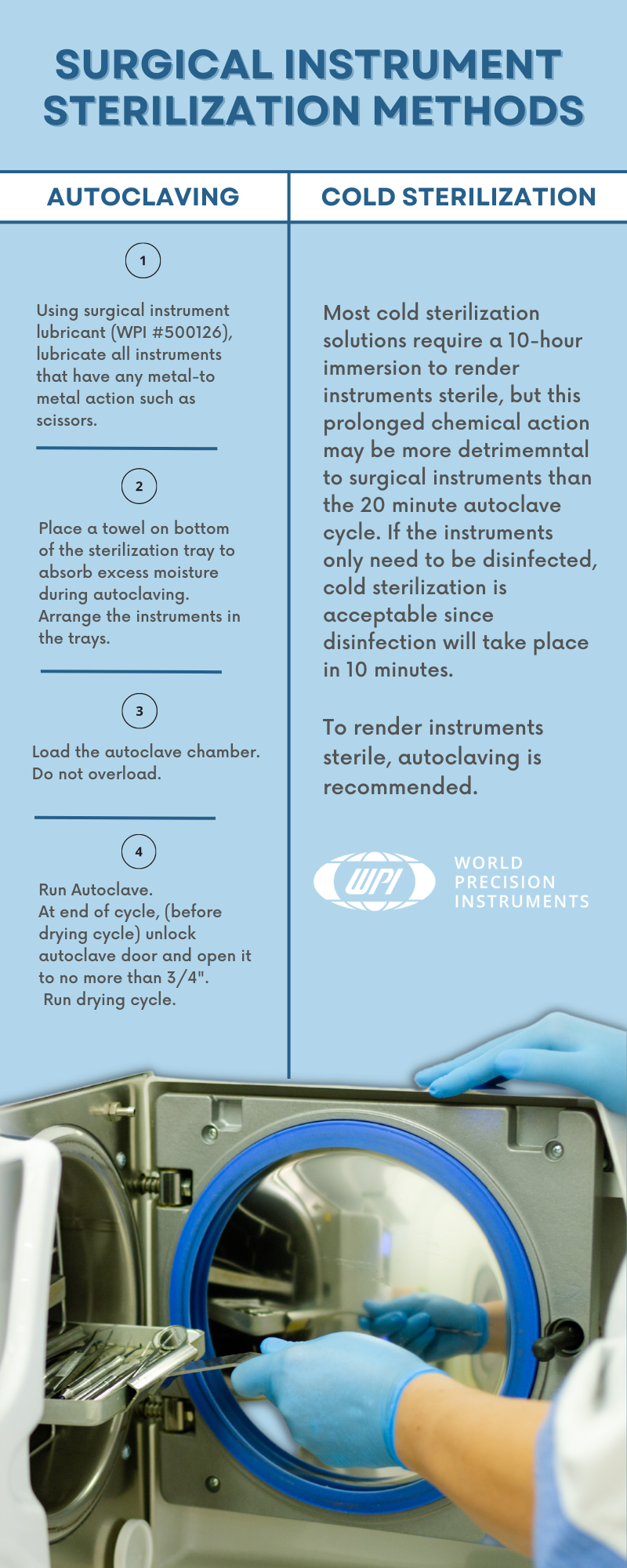
– The intervention, called manual rotation, is performed when the woman is at full cervical dilatation and the fetal position is occiput transverse. The technique used will be at the discretion of the operator and may involve applying pressure to the lambdoid suture or flexion and rotation of the fetal head.
– The comparator is the standard practice of waiting until full dilatation is reached before performing any intervention.
– The primary outcome measure is operative delivery (vacuum, forceps, or caesarean section).
– Secondary outcomes include the rate of caesarean section, serious maternal morbidity or mortality, and serious perinatal and neonatal morbidity and mortality.
– Prolonged second stage of labour is defined differently based on parity and use of epidural analgesia.
– Other outcomes measured include length of second stage, time from randomization to delivery, estimated blood loss, perineal or vaginal trauma requiring suturing, length of hospital stay, and outcomes for operative delivery.
– Secondary outcomes assessed include breastfeeding status, satisfaction with birth, depression, health-related quality of life, and pelvic floor function.
– The sample size for the study is 416 participants, based on power calculations and previous studies.
– The study aims to evaluate the effectiveness of manual rotation in reducing adverse outcomes during transverse arrest.
– The primary outcome measure is serious morbidity and/or mortality, which includes factors such as neonatal injury, low Apgar score, abnormal cord pH levels, birth trauma, seizures, ventilation, tube feeding, NICU admission, and neonatal jaundice.
– Data collection will occur at three possible time points: antenatal, latent phase of labor, or active phase of the first stage of labor.
– Informed consent will be obtained, and participants will be informed of the potential risks of manual rotation.
– An ultrasound will be performed at full dilatation, and the fetal position will be confirmed by a second ultrasound.
– The treatment allocation is recorded on a randomization sheet kept by the investigator.
– The findings are recorded by the investigator.
– The data will be stored securely and checked for accuracy.
– The analysis will be done according to specific guidelines and will include variables such as maternal factors, gestation, and neonatal gender.
– Subgroup analyses will also be performed based on different techniques of manual rotation and operator ability.
– A Data and Safety Monitoring Committee has been established to ensure the safety of the trial participants.
– Any adverse events will be reported to this committee, and serious complications will be referred to them as well.
– The study has received approval from the Ethics Review Committee of the Sydney Local Health District in Sydney, Australia, with the protocol number X110410.
Continue Reading