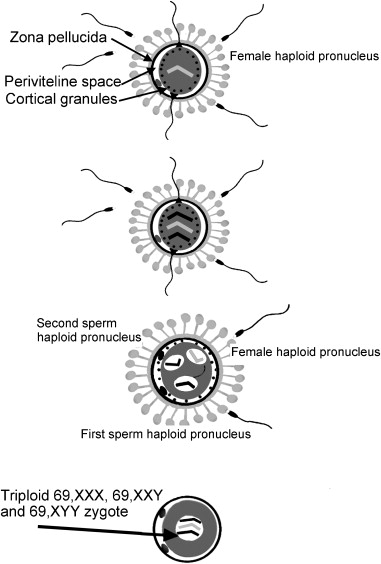
– Molar pregnancy, also known as HM or malignant hydatidiform mole, occurs due to abnormal fertilization of the egg.
– It results in an abnormal fetus and normal growth of the placenta with little or no fetal tissue growth.
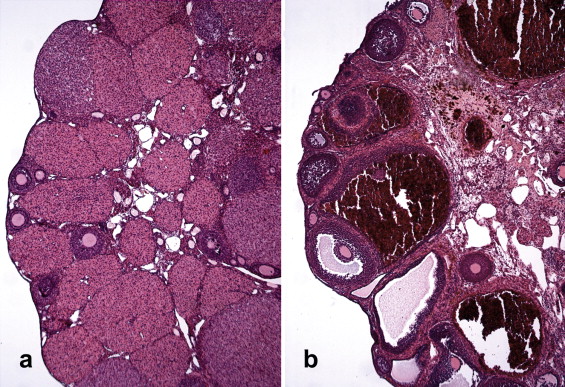
– The placental tissue forms a mass in the uterus with a grape-like appearance on ultrasound, containing small cysts.
– Older women have a higher chance of developing a molar pregnancy.
– A history of molar pregnancy in earlier years is also a risk factor.
– There are two types of molar pregnancy: partial molar pregnancy, where there is an abnormal placenta and some fetal development, and complete molar pregnancy, where there is an abnormal placenta and no fetus.
– There is no known prevention for the formation of these masses.
– Mortality rate from hydatidiform mole is essentially zero due to early diagnosis and appropriate treatment.
– Approximately 20% of women with a complete mole develop a trophoblastic malignancy, which is almost 100% curable.
– Risk factors for malignant disease include advanced maternal age, high levels of hCG (>100,000 mIU/mL), eclampsia, hyperthyroidism, and bilateral theca lutein cysts.
– Predicting who will develop gestational trophoblastic neoplasia is difficult.
– Study suggests that outcomes of subsequent pregnancies in women who have had molar pregnancies are similar to those in the general population.
– Incidence of another molar pregnancy in women with a molar pregnancy is about 1.7%.
– Incidence of stillbirth in subsequent pregnancies in women with gestational trophoblastic neoplasia is 1.3%.
– Women with gestational trophoblastic neoplasia who conceive after chemotherapy have similar obstetric outcomes to those of the general population.
– Following a molar pregnancy, the risk of preterm birth is increased.
– Likelihood of large-for-gestational-age birth and stillbirth is greater if at least one birth occurs between the molar pregnancy and the index birth.
– Risk of adverse maternal outcomes is not increased following molar pregnancy.
– Malignancy is diagnosed in 15-20% of patients with a complete hydatidiform mole and 2-3% of partial moles.
– Lung metastases are found in 4-5% of patients.
– Perforation of the uterus during suction curettage is a potential complication, which may require laparoscopic guidance to complete the procedure.
– Hemorrhage is a common complication during the evacuation of a molar pregnancy, and intravenous oxytocin should be started at the beginning of suctioning.
– Other medications such as Methergine and Hemabate should also be available, and blood for possible transfusion should be readily available.
– Malignant trophoblastic disease develops in 20% of molar pregnancies, so quantitative hCG should be monitored regularly.
– Factors released by the molar tissue could trigger the coagulation cascade, leading to disseminated intravascular coagulopathy (DIC).
– Acute respiratory insufficiency can also occur due to trophoblastic embolism.
– The greatest risk factor for this complication is a larger uterus size compared to the expected gestational age.
Continue Reading