– Prognosis for theca cell tumors (GCTs) is generally very favorable and considered to be tumors of low malignant potential
– Approximately 90% of GCTs are at stage I at the time of diagnosis
– 10-year survival rate for stage I tumors in adults is 90-96%
– GCTs of more advanced stages have 5- and 10-year survival rates of 33-44%
– Overall 5-year survival rates for patients with adult-type GCTs (AGCTs) or juvenile-type GCTs (JGCTs) are 90% and 95-97% respectively
– 10-year survival rate for AGCTs is approximately 76%
– Recurrence rate for AGCTs is 43%
– Average recurrence for AGCTs is approximately 5 years after treatment, with more than half occurring more than 5 years after primary treatment
– Mean survival after recurrence is diagnosed is 5 years for AGCTs
– 10-year overall survival after AGCT recurrence is 50-60%
– JGCTs tend to recur much sooner, with more than 90% of recurrences occurring in the first 2 years
– Tumor stage at initial surgery is the most important prognostic variable
– Other factors predicting survival include early stage disease, age younger than 50 years, high mitotic rates, moderate-to-severe atypia, preoperative spontaneous rupture of the capsule, and tumors larger than 15 cm
– True thecomas have a 5-year survival rate of nearly 100%, but may cause increased morbidity due to estrogen-producing capabilities
– More than 90% of AGCTs and JGCTs are diagnosed before spread occurs outside the ovary
– Five-year survival rates for stage I tumors are usually 90-95%
– AGCTs have a 5-year survival rate of 25-50% for patients with advanced-stage disease
– Late recurrence can occur up to 37 years after diagnosis
– Approximately 20% of GCT patients die from the disease in their lifetime
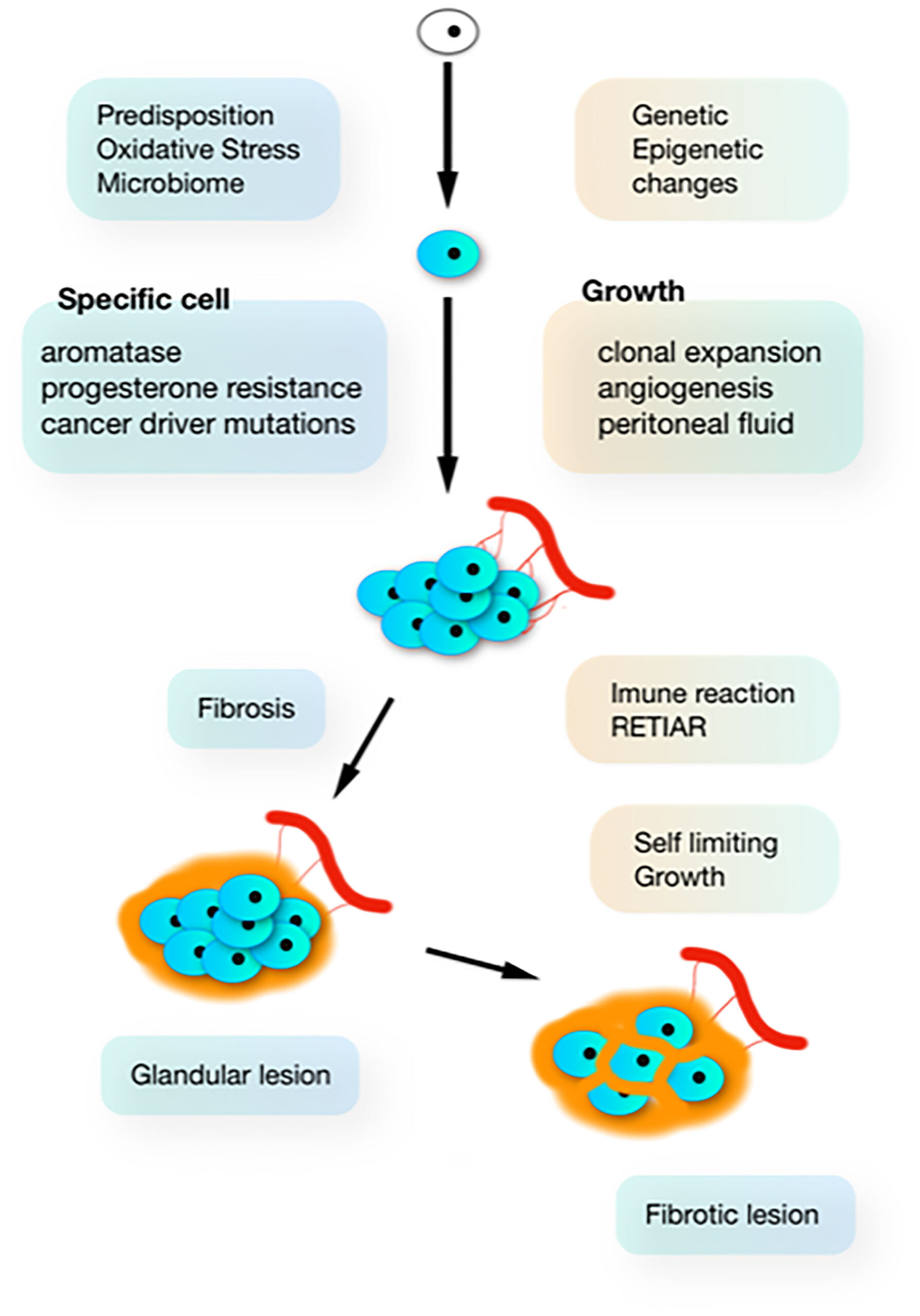
– Morbidity is primarily due to endocrine manifestations of the tumor
– Physical changes caused by high estrogen levels usually regress after tumor removal, but some patients may present with symptoms of androgen excess
– Estrogen production can stimulate the endometrium, leading to endometrial hyperplasia in 30-50% of patients and endometrial adenocarcinoma in 8-33% of patients
– There may also be an increased risk of breast cancer, although it’s difficult to prove a direct correlation
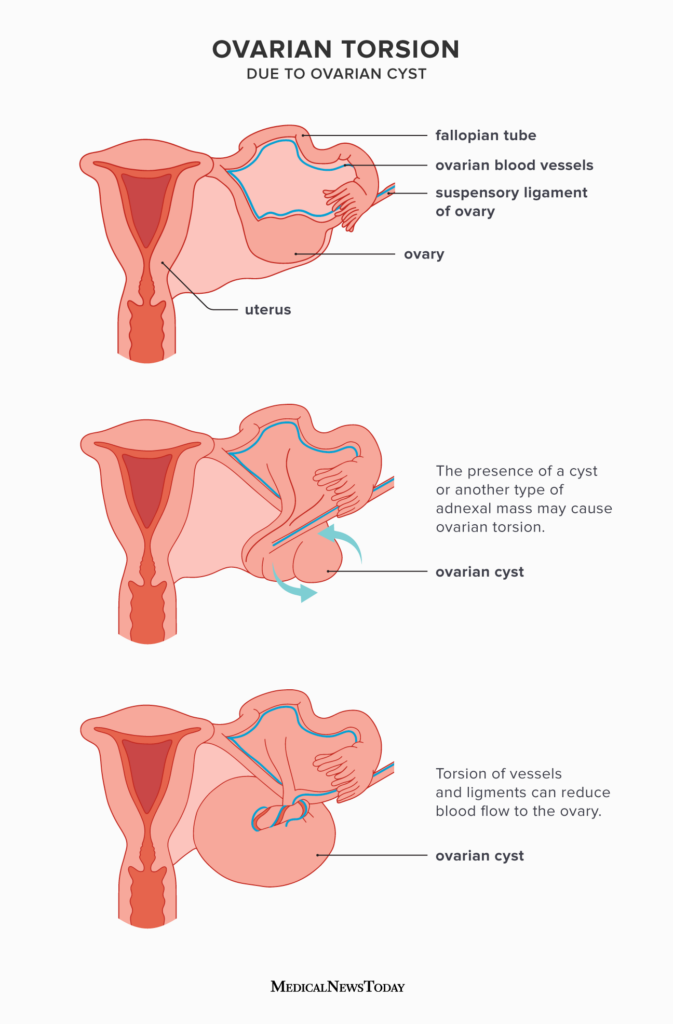
– Acute abdominal symptoms can occur in 10-15% of cases due to rupture, hemorrhage, or ovarian torsion
– Adverse effects from chemotherapy vary depending on the type given
– The standard of care for initial management of GCTs is surgical
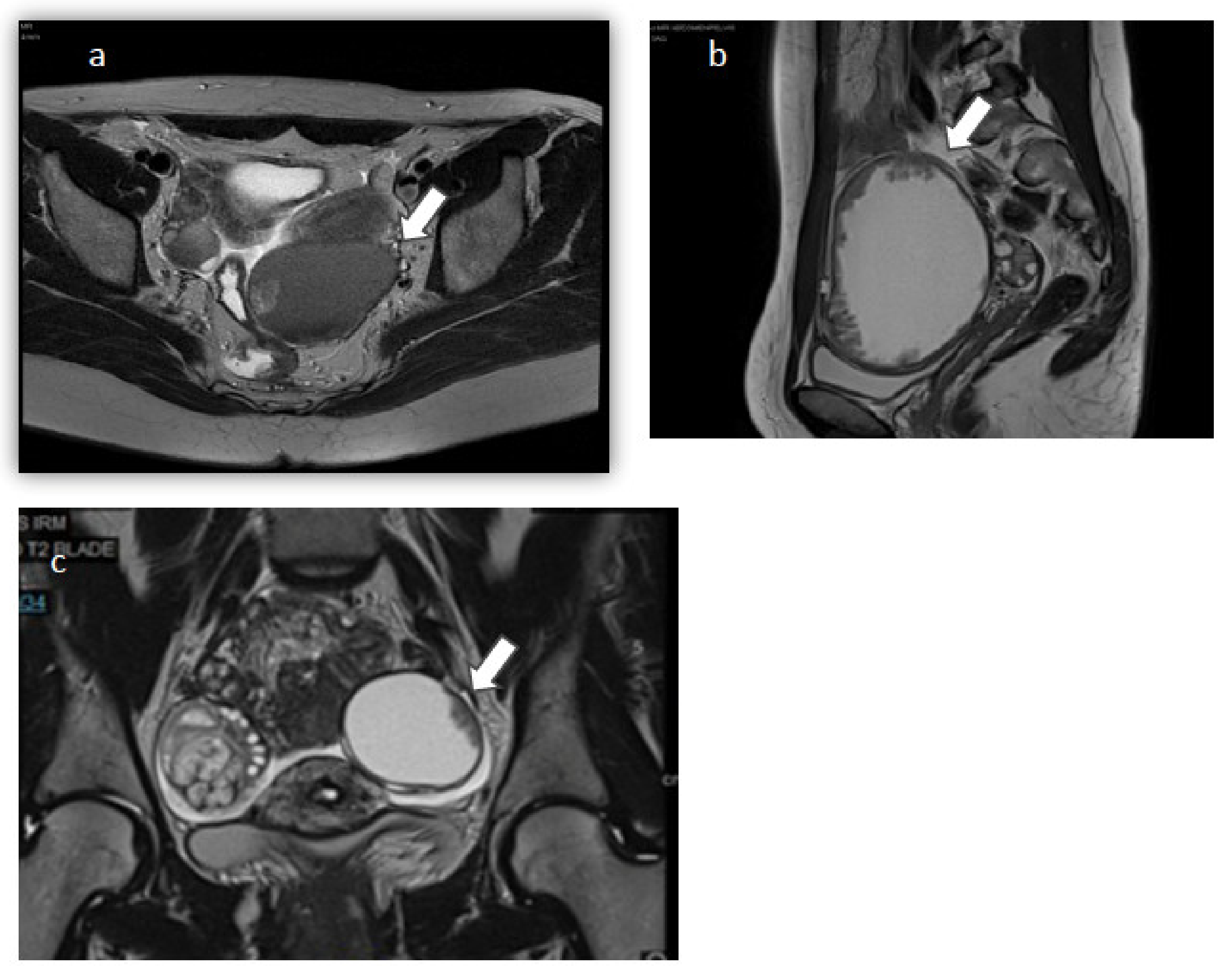
– Preoperative evaluation, including imaging and laboratory studies, helps measure the extent of the disease
– Complete surgical staging is important and involves examination of the pelvic and intra-abdominal structures
– Optimal tumor debulking improves overall survival and decreases recurrences
– In younger patients who desire future fertility, unilateral salpingo-oophorectomy is usually sufficient treatment
– Staging typically involves pelvic washings, lymph node sampling, biopsies, and examination of the contralateral ovary
– The need for lymphadenectomy is being questioned due to the low risk of lymph node metastasis even in advanced stage disease
– Dilatation and curettage should be considered to rule out a neoplastic process of the endometrium in younger patients
– Surgical staging/biopsy based on incidence of microscopic extraovarian disease is important
– For patients who do not require future fertility, surgical therapy should consist of bilateral salpingo-oophorectomy and total abdominal hysterectomy, in addition to staging procedures
– The treatment of recurrent GCTs is not standardized, and surgical debulking may be beneficial if the tumor appears to be focal on imaging studies
– Chemotherapy, radiotherapy, and hormonal treatments have been used with varying success
– The mean survival after a recurrence has been diagnosed is approximately 5 years for adult GCTs.
Continue Reading