Gestational Trophoblastic Tumour: Understanding Diagnosis, Treatment, and Recovery
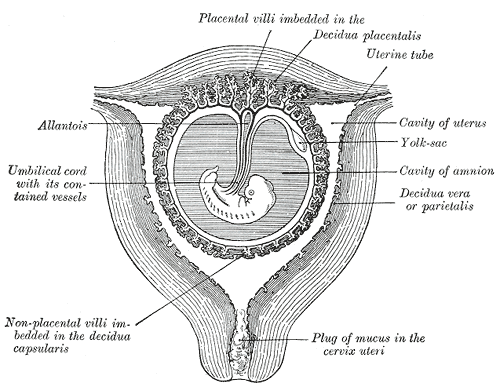
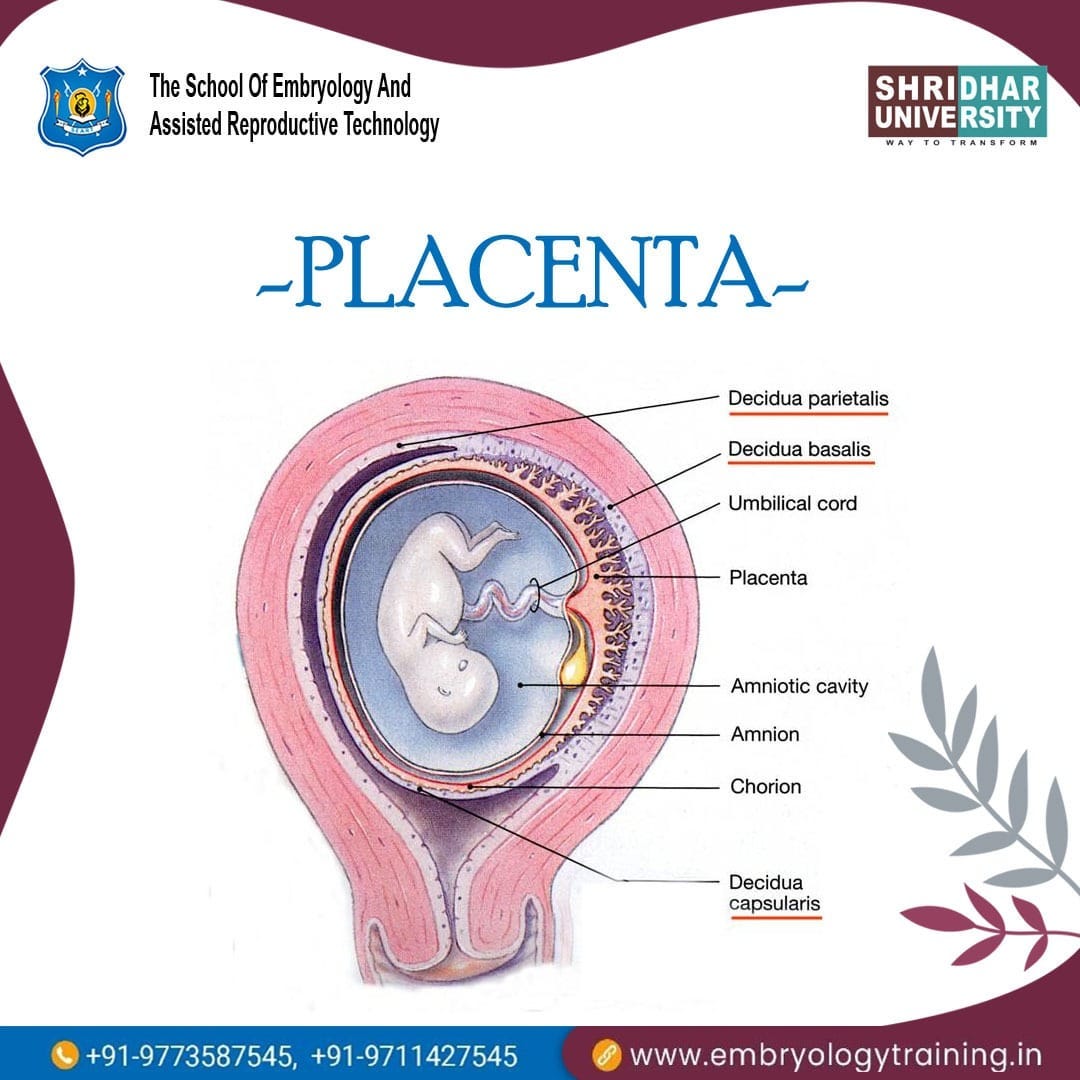
– Gestational trophoblastic tumor is a type of cancer that forms from the cells that would normally develop into the placenta during pregnancy.
– It is rare and usually occurs in women of childbearing age.
– The tumor may be benign or cancerous.
– Symptoms can include abnormal vaginal bleeding, nausea and vomiting, and pelvic pain.
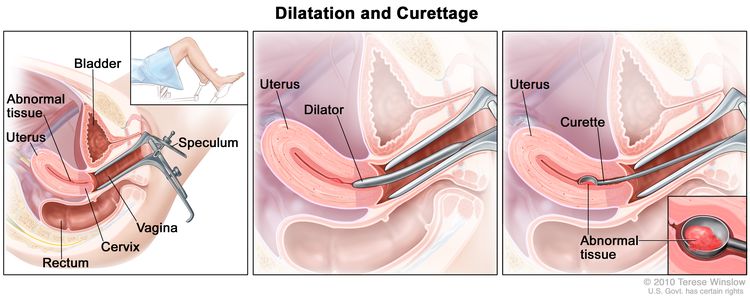
– Treatment options include surgery, chemotherapy, and radiation therapy.
– Clinical trials are being conducted to find new and better ways to treat this type of cancer.
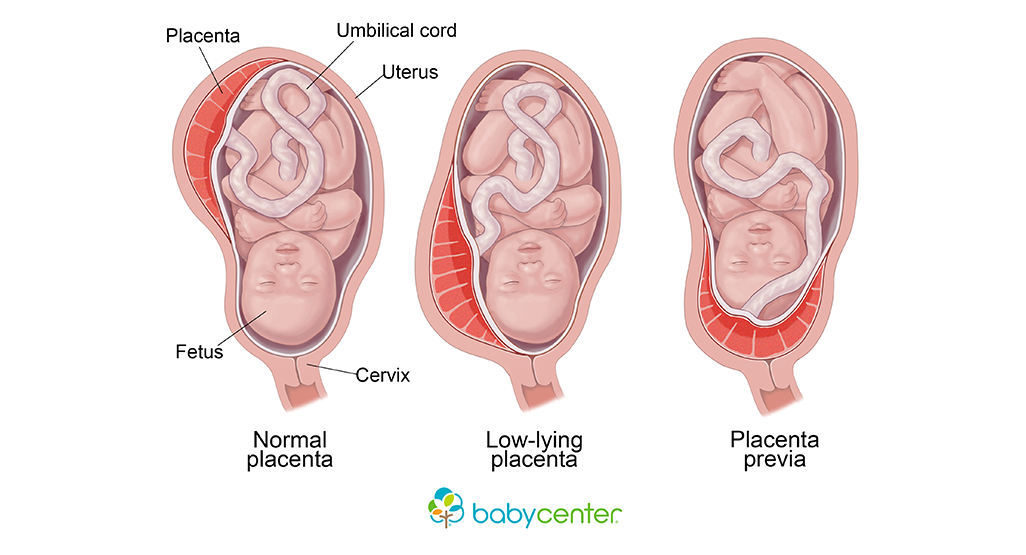
– Gestational trophoblastic disease can occur after any type of pregnancy, including molar pregnancies, pregnancies that end in miscarriage or abortion, and normal pregnancies.
– Gestational trophoblastic disease is rare and can usually be cured with treatment.
– Treatment options for gestational trophoblastic disease include surgery, chemotherapy, and radiation therapy.
– It is important to receive care from a medical team with experience in treating gestational trophoblastic disease.
– The 5-year survival rate for women with low-risk disease is nearly 100%, while the 5-year survival rate for women with high-risk disease is about 90%.
– Gestational trophoblastic disease can sometimes spread to other parts of the body, such as the lungs, making treatment more difficult.