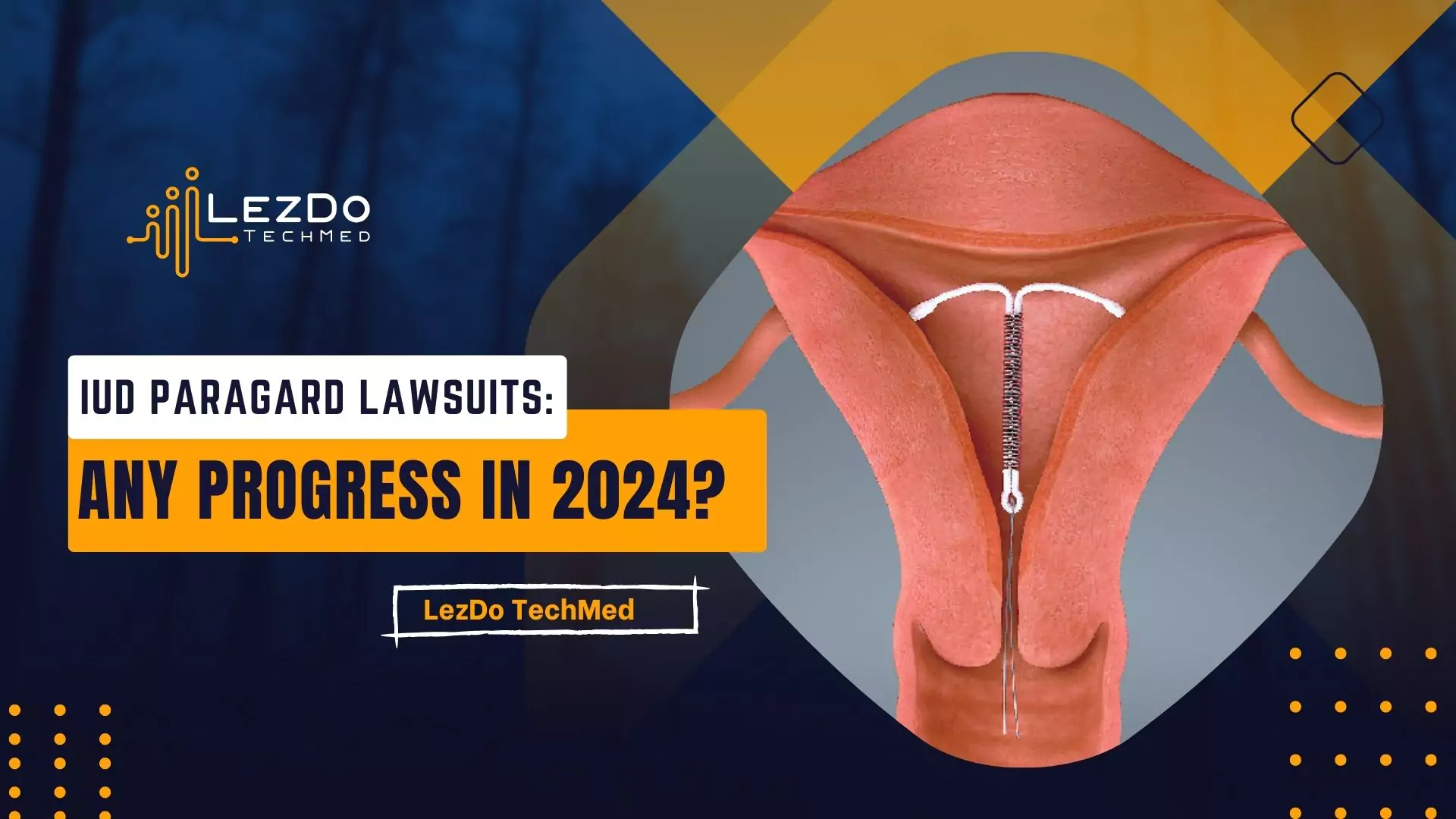
– IUD can be partially expelled from the uterus, and the user may not be aware of it.
– The rates of IUD expulsion range between 0.05% and 8%.
– Factors that can affect the possibility of expulsion include age, pregnancy history, time since insertion, and insertion technique.
– Rates of expulsion are higher during the first three months and during periods.
– If experiencing severe pain, abnormal bleeding or discharge, or fever, it is recommended to make an appointment with a healthcare provider.
– Discomfort in the first few days after insertion is normal, but worsening or persistent pain may require medical attention.
– The article provides information about what to do if an IUD (intrauterine device) has been expelled from the body.
– If the IUD is not in its proper place, it may not effectively prevent pregnancy.
– It advises contacting a healthcare provider as soon as possible and making an appointment if there is severe pain, inability to find the strings of the IUD, abnormal string length, or if the IUD can be felt poking out.
– The article recommends a routine check-up after six weeks of IUD insertion to ensure good health.
– The chance of IUD expulsion happening again is slightly higher for women who have experienced it before.
– If an intrauterine device (IUD) falls out, do not try to put it back in and contact a healthcare provider immediately.
– IUD is a small, T-shaped device that provides long-term and effective birth control.
– There are two types of IUDs: hormonal IUDs that release progestin and last three to five years, and copper IUDs that start working immediately and can remain effective for up to 10 years.
– The IUD is inserted by a healthcare provider, usually during the period, and takes around five to 15 minutes.
– Mild discomfort and cramping may be experienced during and after the insertion.
– Reasons for an IUD falling out include being under 20 years old, not having been pregnant, recent childbirth, abortion, experiencing heavy, painful, or prolonged periods, or being on your period.
– The reasons for IUD expulsion are unclear but not associated with exercise, sex, or going to the bathroom.
– Women can check their IUD to ensure it is in place and not starting to fall out.
– Signs that indicate an IUD has moved or been expelled include shorter or longer strings, inability to find the strings, feeling the IUD against the cervix, pain, discomfort, severe cramps, heavy or abnormal bleeding, unusual vaginal discharge, and fever if an infection has occurred.
– Backup birth control should be used, such as condoms, as pregnancy can occur after expulsion.
– The article also suggests alternative forms of birth control such as the pill, patch, ring, and shot, as well as barrier methods.
– Additionally, it mentions other side effects of IUDs, including cramping, irregular bleeding, longer and heavier periods, premenstrual syndrome symptoms, pelvic infection, and rarely, perforation of the uterus.
– IUDs do not protect against sexually transmitted infections.
Continue Reading