– Endometriosis is a disease in which tissue similar to the lining of the uterus grows outside the uterus.
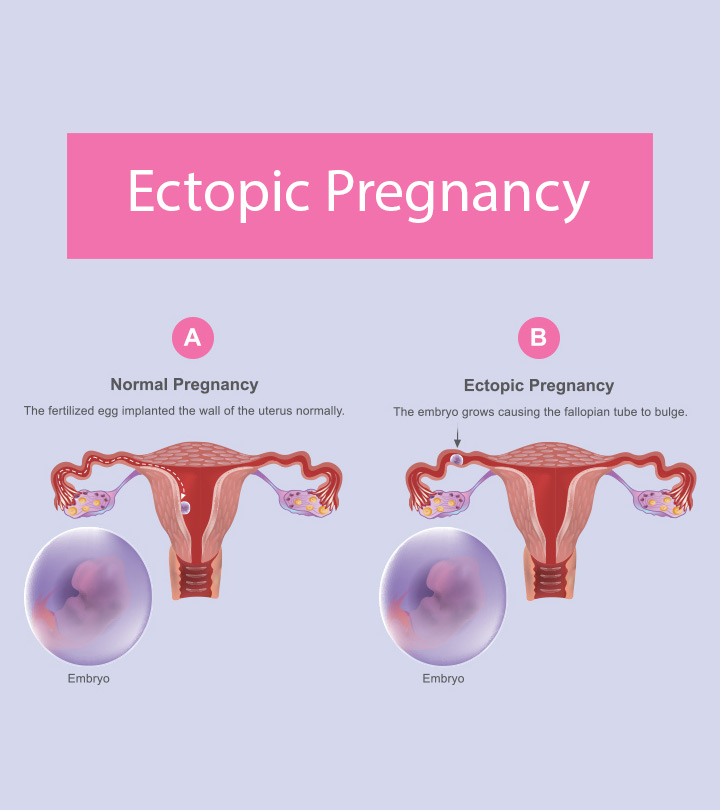
– It can cause severe pelvic pain and make it harder to get pregnant.
– The cause of endometriosis is unknown, and there is no known way to prevent it.
– There is no cure for endometriosis, but its symptoms can be treated with medicines or surgery.
– It causes a chronic inflammatory reaction and can result in the formation of scar tissue.
– Different types of endometriosis lesions have been described, including superficial, cystic ovarian, and deep endometriosis.
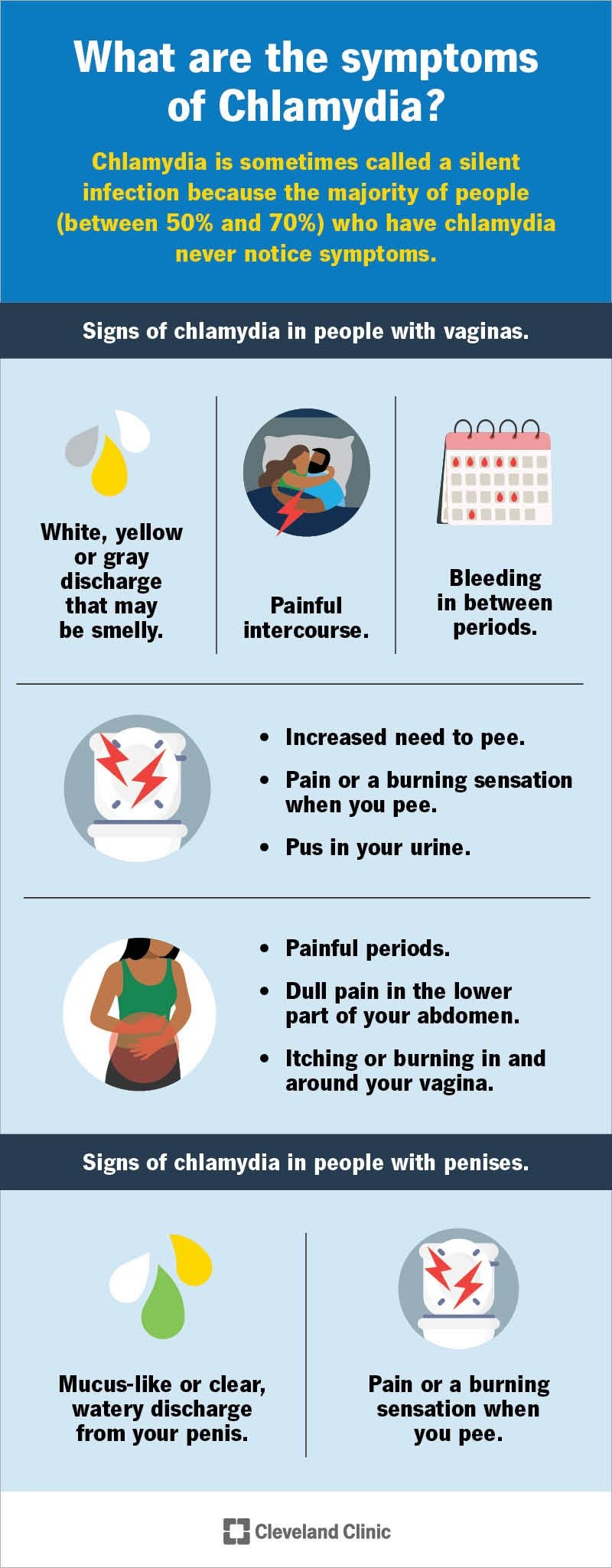
– Symptoms of endometriosis include severe pelvic pain, pain during sex or when using the bathroom, trouble getting pregnant, heavy bleeding, bloating, fatigue, depression, and anxiety.
– Retrograde menstruation, cellular metaplasia, and stem cells are thought to contribute to the development of endometriosis.
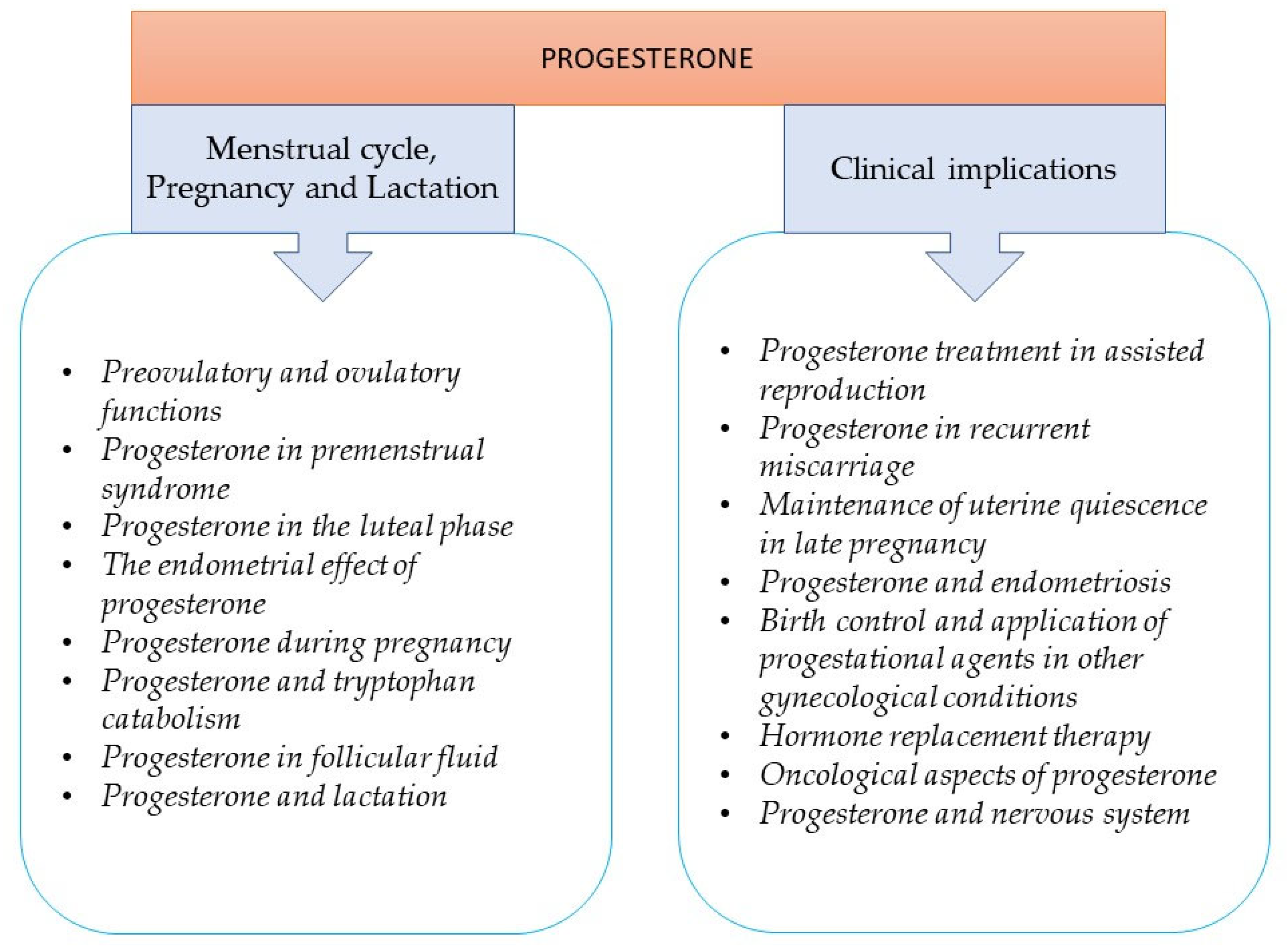
– Estrogen is known to be involved in endometriosis, but the relationship is complex.
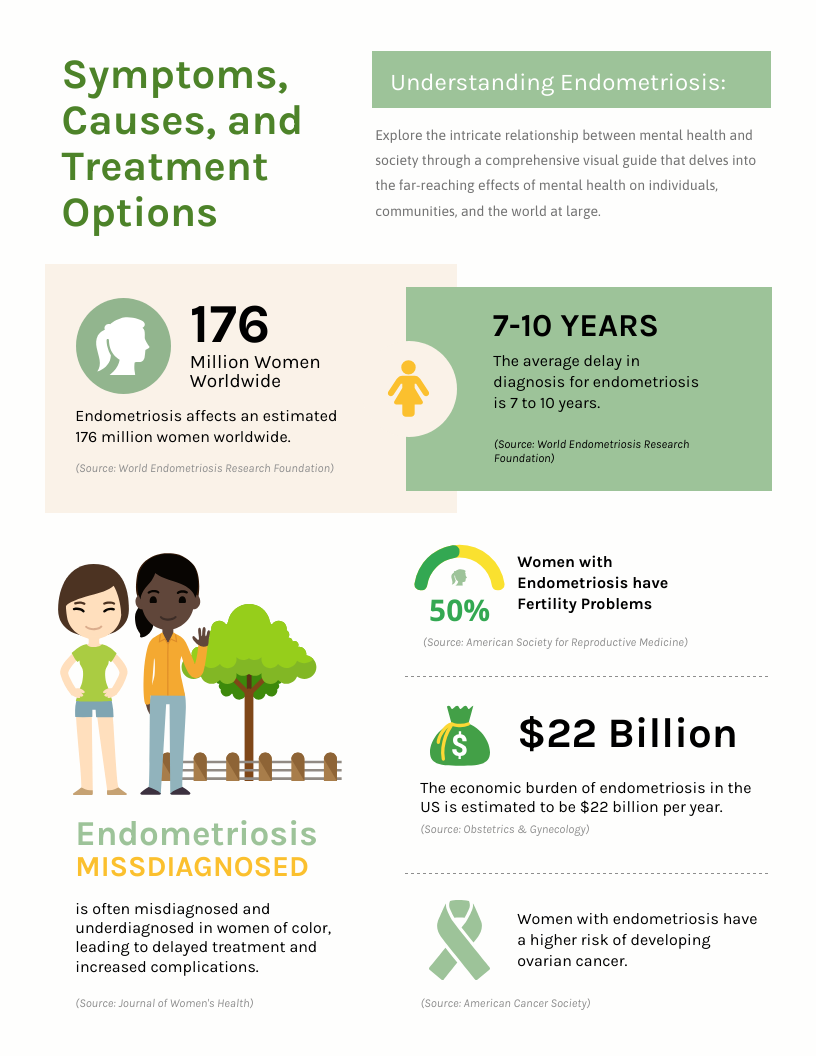
– Endometriosis has significant social, public health, and economic implications.
– It can decrease quality of life due to severe pain, fatigue, depression, anxiety, and infertility.
– Pain can prevent individuals from going to work or school.
– Painful sex due to endometriosis can impact sexual health.
– There is currently no known way to prevent endometriosis.
– Early diagnosis and management can slow or halt the progression of the disease.
– Several screening tools and tests have been proposed but none are validated to accurately identify the disease.
– Ultrasonography or MRI can be used to detect certain forms of endometriosis.
– Histologic verification through surgical/laparoscopic visualization can help confirm diagnosis.
– Treatments for endometriosis vary based on symptom severity and desire for pregnancy.
– No treatments cure the disease.
– Non-steroidal anti-inflammatory drugs (NSAIDs) and painkillers like ibuprofen can be used to treat pain.
– Hormonal medicines and contraceptive methods can help control pain.
– Fertility medicines and procedures may be used for those having difficulty getting pregnant.
– Surgery is sometimes used to remove endometriosis lesions and scar tissue.
– Treatment options depend on individual preferences, effectiveness, side effects, safety, cost, and availability.
– Raising awareness can lead to early diagnosis and treatment.
– Hormonal management can have adverse side effects and may not be suitable for individuals with endometriosis who want to get pregnant.
– Success in reducing pain symptoms and increasing pregnancy rates through surgery depends on the severity of the disease.
– Lesions may recur even after successful treatment, and pelvic floor muscle abnormalities can contribute to chronic pelvic pain.
– Physiotherapy and complementary treatments may benefit patients with secondary changes in the pelvis and central sensitization.
– Treatment options for infertility caused by endometriosis include surgical removal, ovarian stimulation with intrauterine insemination, and in vitro fertilization.
– Lack of awareness among the general public and healthcare providers can lead to a delay in diagnosis.
– Limited awareness of endometriosis among primary healthcare providers can result in a lack of medical treatment for symptomatic management.
– Access to specialized surgery is sub-optimal in many countries, particularly low and middle-income countries.
– Screening and accurate prediction tools for endometriosis are lacking.
– Non-invasive diagnostic methods and medical treatments that do not prevent pregnancy are needed.
– WHO recognizes the impact of endometriosis on sexual and reproductive health and aims to stimulate effective policies and interventions globally.
– WHO partners with various stakeholders, including research institutions and patient support groups, to address endometriosis.
– WHO collaborates with stakeholders to collect and analyze endometriosis prevalence data for decision-making.
Continue Reading