The claustrum is a thin sheet of neurons and supporting glial cells in the brain that connects to the cerebral cortex and subcortical regions. It is located between the insular cortex and putamen. The claustrum is considered to be the most densely connected structure in the brain and is hypothesized to integrate various sensory inputs into one experience. It may also play a role in salience processing and attention. The claustrum is made up of different cell types, with the principal cell type being the Golgi type I neuron. It is believed to synchronize activity in different parts of the brain and support consciousness. The claustrum may also differentiate between relevant and irrelevant information. Its precise boundaries are still debated.
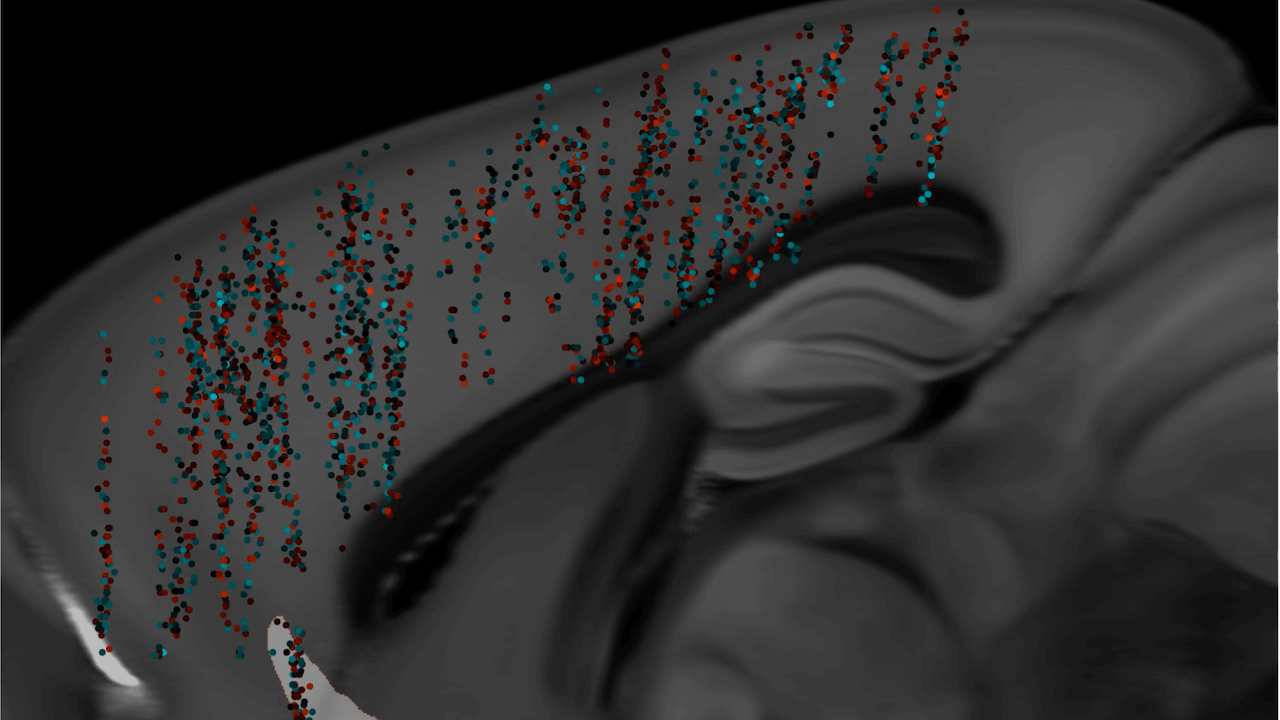
The claustrum is a brain structure that has extensive connections to both cortical and subcortical regions. It is highly connected to thalamic nuclei, the basal ganglia, and various regions of the cortex. The claustrum is the most highly connected structure per regional volume in the brain and may serve as a hub to coordinate activity of cerebral circuits. It is involved in processing sensory information and the physical and emotional state of an animal. Inputs to the claustrum are organized by modality, including prefrontal, visual, auditory, and somatomotor processing areas. The claustrum possesses a distinct topological organization for each sensory modality and has dense connectivity with frontal cortices. Local connectivity within the claustrum is dominated by feed-forward disynaptic inhibition. Excitatory claustrum neurons form synapses across the anteroposterior axis and are biased toward neurons that do not share projection targets. Overall, these findings suggest that the claustrum is capable of performing local transformations of diverse input information from across the brain.
The claustrum is a part of the brain composed of various cell types. Excitatory cells in the claustrum project to different brain regions. Inhibitory neurons make up 10%-15% of the claustrum and express parvalbumin, somatostatin, or vasoactive intestinal peptide. The claustrum can be identified by its prominent plexus of parvalbumin-positive fibers. Different methods, such as electrophysiological, morphological, genetic, and connectomic approaches, have been used to study the claustrum in mice. The claustrum has widespread connectivity with cortical components associated with consciousness and sustained attention. It acts as a “conductor” in coordinating the function of all connections. The claustrum has reciprocal connections to the prefrontal cortex, visual, auditory, sensory, and motor regions. It is proposed that the claustrum functions in the gating of selective attention, selectively controlling input from different modalities. The claustrum may also implement resistance to certain inputs to prevent distraction. The claustrum integrates various sensory and motor modalities from different parts of the cortex to facilitate consciousness.
Functional imaging studies show dampened activity in the claustrum when anesthetized versus awake in rats. The claustrum has strong functional connections with the contralateral hemisphere’s claustrum, the mediodorsal thalamus, the medial prefrontal cortex, and surrounding and distant cortical areas.
The claustrum is a region in the brain that plays a role in integrating different modalities, such as sensory and motor functions. It has been shown to have connections with various parts of the cortex and is involved in processes such as spatial navigation and slow-wave sleep. The claustrum also has the ability to select between task relevant and irrelevant information for directed attention. It receives input from visual and auditory centers and can be activated by unexpected stimuli. Electrical stimulation of the claustrum can cause inhibition, leading to a blank stare and unresponsiveness. Salvinorin A, a hallucinogenic compound, can bind to Kappa Opioid Receptors in the claustrum, inducing a loss of awareness and synesthesia. High frequency stimulation of the claustrum in cats and humans has been shown to induce a decrease in awareness and consciousness.
MRI studies have also shown increased signal intensity within the claustrum. The claustrum has been associated with status epilepticus, where epileptic seizures occur without recovery of consciousness in between events. Increased signal intensity in the claustrum is associated with Focal dyscognitive seizures, which impair awareness or consciousness without convulsions. Studies have shown that the claustrum is active during REM sleep and may play a role in spatial memory consolidation. Damage to the claustrum is associated with duration of loss of consciousness in traumatic brain injuries. Stimulation of the extreme capsule, near the claustrum, can disrupt consciousness in a case study. Decreased grey matter volume in the left claustrum is associated with greater delusions in schizophrenia. Lesions to both claustrums would be needed to cause total loss of function. Electrical stimulation of the claustrum did not disrupt consciousness in a study of five patients. Damage to the claustrum may mimic other diseases or mental disorders.
Summary:
The claustrum, a region in the brain, has been found to be involved in various neurological conditions. In autism, a decrease in grey matter volume in the claustrum and insula is associated with an increase in positive symptoms. For epilepsy, increased claustral signal intensity has been observed in MRI scans of diagnosed individuals. Electrical stimulation of the claustrum has been found to disrupt consciousness, while lesions in the claustrum can lead to a loss of consciousness. However, a recent study found no disruption of consciousness with electrical stimulation. Artificial activation of the claustrum can silence brain activity across the cortex. Lesions in the claustrum have been identified as the likely origin of parkinsonism across different conditions. In mice, suppression of the claustrum attenuates anxiety and stress and increases chronic stress-resistance. The claustrum has extensive connections throughout the cortex and with sensory and motor regions in animals. The article discusses the anatomy and function of the claustrum in cats, rodents, and monkeys. In cats, high-frequency stimulation of the claustrum can alter motor activity and induce changes in awareness. The claustrum in cats responds to sensory stimuli and is connected to the motor, somatosensory, visual, and auditory cortex. Sensory input in cats is segregated based on modalities, with a preference for peripheral sensory information. In rodents, the claustrum has distinct patterning of connectivity with different cortical areas and plays specialized roles in cortical processing. In mice, inhibitory interneurons strongly modulate the activity of the claustrum and synchronize activity of claustrocortical projections to influence brain rhythms and coordinated activity of different cortical regions. In monkeys, the claustrum has widespread connections. The claustrum has connections with various cortical regions including the frontal lobe, visual cortex, temporal cortex, parieto-occipital cortex, and somatosensory areas. It also projects towards subcortical areas such as the amygdala, caudate nucleus, and hippocampus. The claustrum may have bi-directional connections with motor structures in the cortex. 70% of movement neurons in the dorsocaudal claustrum are non-selective and can fire for various types of movements, while the remaining neurons are more specific and only fire for one type of movement.
Continue Reading