The Irregular Shedding of Endometrium: Understanding Menstrual Cycles
– Abnormal uterine bleeding refers to heavy or unusual bleeding from the uterus.
– Symptoms include vaginal bleeding between periods and extremely heavy bleeding during periods.
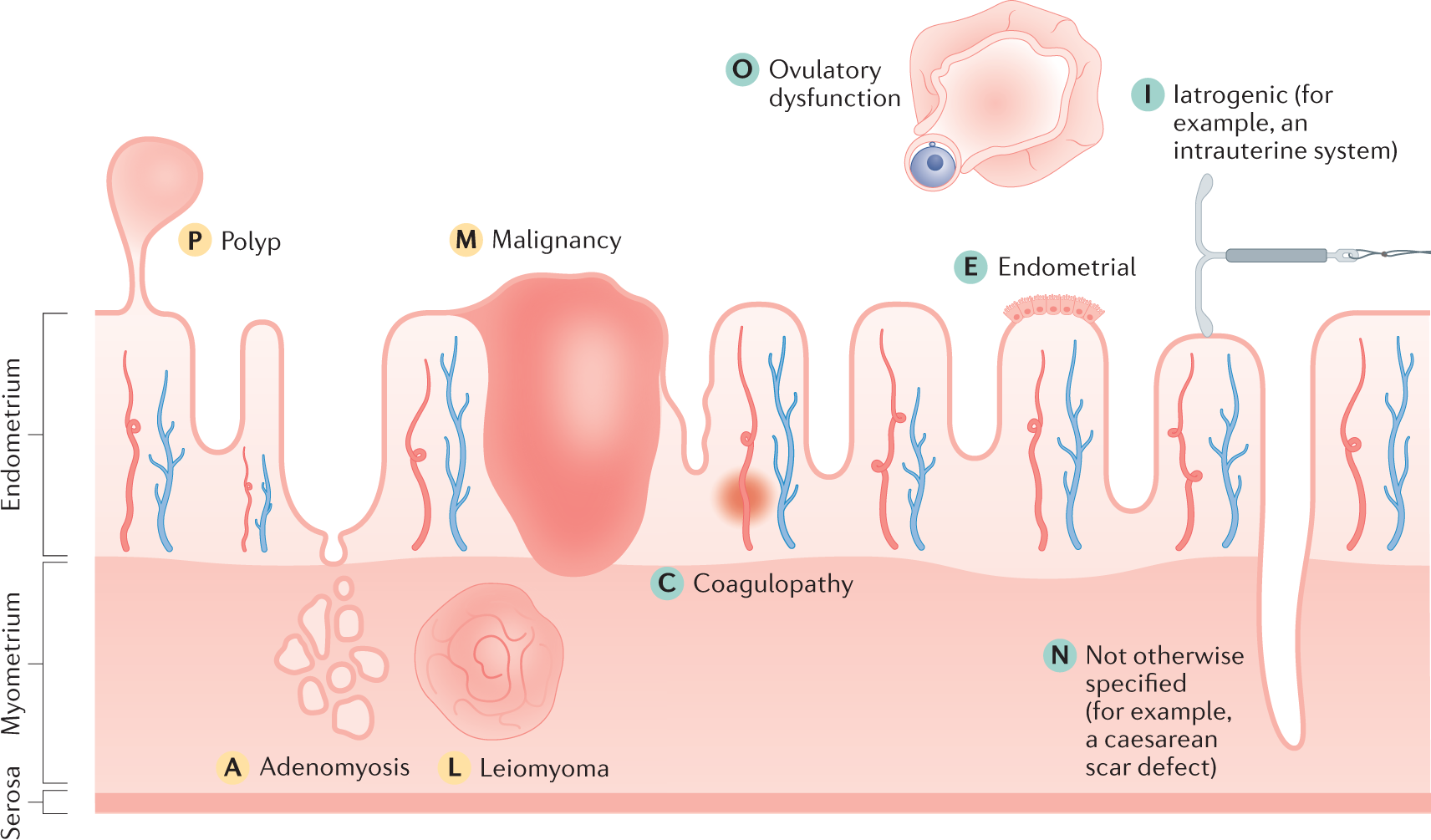
– Abnormal uterine bleeding can be caused by hormonal imbalances, pregnancy, polycystic ovary syndrome (PCOS), growths in the uterus (polyps or fibroids), infection, liver/kidney/thyroid disease, bleeding disorder, or cancer of the uterus/cervix.
– In teenagers and young adults, common causes include pregnancy, certain birth control methods, and hormonal imbalances.
– In the 40s and early 50s, abnormal uterine bleeding can be caused by a lack of ovulation, thickening of the uterine lining, or uterine cancer.
– Hormone replacement therapy is a common cause of uterine bleeding after menopause. There are various causes of abnormal uterine bleeding, including endometrial and uterine cancer. It is more common in older individuals. Other problems can also cause bleeding after menopause. It is important to consult a doctor if experiencing bleeding after menopause. Diagnosis may involve pregnancy tests, blood tests, ultrasound exams, endometrial biopsies, and hysteroscopy. Most causes of abnormal uterine bleeding are not preventable, but maintaining a healthy weight can help in some cases. Treatment options include birth control pills and intrauterine devices.
– One type of hormonal birth control, known as intrauterine devices (IUDs), can cause abnormal bleeding.
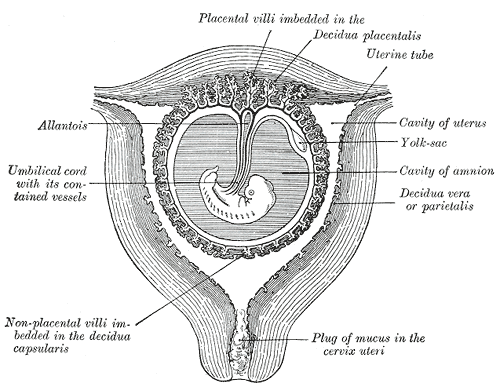
– A dilation and curettage (D&C) procedure involves stretching the cervix and using a surgical tool to scrape away the lining of the uterus. This procedure can be used to both diagnose and treat abnormal bleeding.
– Hysterectomy, the surgical removal of the uterus, stops menstrual bleeding and prevents pregnancy. It is a major surgery that requires general anesthesia and a hospital stay.
– Endometrial ablation is a surgical procedure that destroys the lining of the uterus but does not remove the uterus itself. It can often stop menstrual bleeding.
– Living with abnormal uterine bleeding can have a negative impact on daily life, causing anxiety and limiting activities.
– Ibuprofen can be taken during periods to help reduce pain and cramping.
– It is important to ensure adequate iron intake to prevent anemia.
– Questions to ask a doctor include the likely cause of abnormal bleeding, the seriousness of the condition, recommended treatment options, and the impact on future pregnancy chances.
– Doctors can determine if a woman has endometrial hyperplasia through medical history, symptoms, physical exam, and diagnostic tests.
– Medical history includes asking about irregular menstrual bleeding, menstrual history, pregnancy history, and medication usage.
– A pelvic exam may be normal as endometrial hyperplasia doesn’t cause physical changes to the reproductive system.
– Additional tests may be recommended, such as a transvaginal ultrasound to check the thickness of the uterine lining.
– If the uterine lining is too thick, a biopsy may be offered to diagnose the condition.
– In some cases, a procedure called dilation and curettage (D&C) and hysteroscopy may be performed.
– Results of the biopsy may show normal, abnormal non-cancerous, abnormal precancerous, or abnormal cancerous uterine lining cells.
– Abnormal findings that are non-cancerous and precancerous indicate endometrial hyperplasia.