Rare and enigmatic, theca cell tumors loom in the realm of medical mysteries.
With a prognosis as intriguing as their name, these tumors have managed to baffle doctors and captivate researchers.
Unravel the enigma as we delve into the world of theca cell tumors, where the line between survival and recurrence is as thin as a surgical scalpel.
theca cell tumor
Theca cell tumors, also known as granulosa cell tumors (GCTs), generally have a very favorable prognosis and are considered tumors of low malignant potential.
The majority of GCTs are diagnosed at stage I, and the 10-year survival rate for stage I tumors in adults is 90-96%.
However, more advanced stages of GCTs have lower survival rates, with 5- and 10-year rates ranging from 33-44%.
The overall 5-year survival rates for adult-type GCTs (AGCTs) and juvenile-type GCTs (JGCTs) are 90% and 95-97% respectively.
AGCTs have a 10-year survival rate of approximately 76%.
Recurrence rates for AGCTs are 43%, with the average recurrence occurring around 5 years after treatment.
The 10-year overall survival after AGCT recurrence is 50-60%.
In contrast, JGCTs tend to recur much sooner, with more than 90% of recurrences occurring in the first 2 years.
Overall, factors such as tumor stage, early stage disease, age younger than 50 years, mitotic rates, atypia, rupture of the capsule, and tumor size can impact prognosis.
Morbidities associated with GCTs include endocrine manifestations, estrogen-related complications such as endometrial hyperplasia and adenocarcinoma, and acute abdominal symptoms.
Surgical intervention is the primary treatment for GCTs, with optimal tumor debulking improving overall survival and decreasing recurrences.
For younger patients desiring fertility, unilateral salpingo-oophorectomy may be sufficient, while bilateral salpingo-oophorectomy and total abdominal hysterectomy are recommended for patients not requiring future fertility.
The treatment of recurrent GCTs varies, with surgical debulking and other modalities such as chemotherapy, radiotherapy, and hormonal treatments utilized.
The mean survival after recurrence for adult GCTs is approximately 5 years.
Key Points:
- Theca cell tumors, also known as granulosa cell tumors, have a favorable prognosis and are considered tumors of low malignant potential.
- The majority of GCTs are diagnosed at stage I, with a 10-year survival rate of 90-96% in adults.
- More advanced stages of GCTs have lower survival rates, ranging from 33-44% at 5 and 10 years.
- Adult-type GCTs have a 5-year survival rate of 90% and a 10-year rate of 76%.
- Recurrence rates for AGCTs are 43%, with the average recurrence occurring around 5 years after treatment.
- Juvenile-type GCTs tend to recur much sooner, with over 90% of recurrences happening within the first 2 years.
theca cell tumor – Watch Video
💡
Pro Tips:
1. Theca cell tumors are a rare type of ovarian tumor that usually affect young women of reproductive age.
2. Despite being rare, theca cell tumors are usually benign and do not spread to other parts of the body.
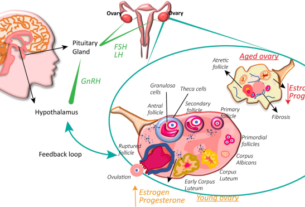
3. These tumors develop from the cells that surround and support the eggs in the ovaries, known as theca cells.
4. Theca cell tumors can sometimes produce excess hormones, leading to symptoms such as irregular periods, acne, and abnormal hair growth.
5. In some cases, theca cell tumors can be associated with other ovarian conditions, like polycystic ovary syndrome (PCOS).
1. Prognosis For Theca Cell Tumors (GCTs)
The prognosis for theca cell tumors, also known as granulosa cell tumors (GCTs), is generally very favorable. These tumors are considered to be of low malignant potential, meaning that they are less likely to spread aggressively and cause significant harm. Approximately 90% of GCTs are at stage I at the time of diagnosis, indicating that the tumor is confined to the ovary and has not spread to other parts of the body.
2. Stage I Survival Rates In Adults
The 10-year survival rate for stage I GCTs in adults is high, ranging from 90% to 96%. This implies that the majority of patients with stage I tumors have a good chance of living at least 10 years after their initial diagnosis. Stage I tumors are the earliest stage of GCTs and have the best prognosis because they are localized to the ovary and have not spread to other organs.
3. Survival Rates For Advanced Stage GCTs
GCTs at more advanced stages have significantly lower survival rates. For instance, GCTs at stages II, III, and IV have 5-year survival rates ranging from 33% to 44%. This pattern continues with 10-year survival rates, indicating that as the tumor progresses and spreads to other parts of the body, the chances of long-term survival decrease significantly.
4. Survival Rates For Adult-Type GCTs (AGCTs) And Juvenile-Type GCTs (JGCTs)
The overall 5-year survival rates for patients with adult-type GCTs (AGCTs) and juvenile-type GCTs (JGCTs) are high. AGCTs have a 5-year survival rate of 90%, while JGCTs have a 5-year survival rate of 95-97%. These figures indicate that the majority of patients with either type of GCT have a good prognosis and are likely to survive at least 5 years after their diagnosis.
5. Recurrence Rates And Timing For AGCTs
AGCTs, or Adult Granulosa Cell Tumors, are known to have a considerably high recurrence rate of 43%. Recurrence specifically refers to the reappearance of the tumor following the initial treatment. On average, AGCTs tend to recur around 5 years after the initial treatment, with over 50% of recurrences happening more than 5 years after the primary treatment. These findings underscore the critical significance of long-term follow-up and surveillance for patients with AGCTs. Timely detection and management of recurrences are crucial in ensuring effective treatment outcomes.
6. Prognostic Variables For AGCT Survival
Several variables can help predict the survival of patients with AGCTs. The tumor stage at initial surgery is the most important prognostic variable. Other factors that predict better survival include early stage of disease, age younger than 50 years, high mitotic rates (indicating faster cell division), moderate-to-severe atypia (abnormal cellular features), preoperative spontaneous rupture of the capsule, and tumors larger than 15 cm.
These factors can aid in assessing the prognosis of AGCTs and guiding treatment decisions.
- Tumor stage at initial surgery
- Early stage of disease
- Age younger than 50 years
- High mitotic rates (indicating faster cell division)
- Moderate-to-severe atypia (abnormal cellular features)
- Preoperative spontaneous rupture of the capsule
- Tumors larger than 15 cm
7. Survival Rates And Morbidity For True Thecomas
True thecomas are a subtype of GCTs (granulosa cell tumors) with a remarkable 5-year survival rate of almost 100%. However, their estrogen-producing capabilities can give rise to increased morbidity. Morbidity refers to the impact of illness on overall health and well-being. In the case of true thecomas, the elevated estrogen levels can lead to physical changes, such as endometrial hyperplasia (thickening of the uterus lining) in 30-50% of patients and endometrial adenocarcinoma (uterine lining cancer) in 8-33% of patients. Furthermore, although establishing a direct correlation is challenging, there may be an increased risk of breast cancer associated with true thecomas.
8. Spread Of GCTs Outside The Ovary
More than 90% of AGCTs and JGCTs are diagnosed before spread occurs outside the ovary. This suggests that GCTs have a propensity to remain localized within the ovary, making early detection and treatment critical for optimal outcomes. When GCTs do spread outside the ovary, the prognosis becomes less favorable, and survival rates decrease accordingly.
9. Morbidity And Endocrine Manifestations Of GCTs
The primary source of morbidity in patients with GCTs is the endocrine manifestations of the tumor. GCTs have the potential to produce hormones such as estrogen and androgens, which can lead to various symptoms and complications. Physical changes caused by high estrogen levels, such as breast enlargement and changes in menstrual patterns, usually regress after tumor removal. However, some patients may present with symptoms of androgen excess, such as hirsutism (excessive hair growth), male-pattern baldness, or voice deepening.
These endocrine effects can impact a patient’s quality of life and require ongoing management and monitoring.
- Estrogen and androgens are produced by GCTs
- Breast enlargement and changes in menstrual patterns are common physical changes
- Symptoms of androgen excess include hirsutism, male-pattern baldness, and voice deepening
“These endocrine effects can impact a patient’s quality of life and require ongoing management and monitoring.”
10. Surgical Management And Treatment Options For GCTs
The standard of care for initial management of GCTs is surgical intervention. Preoperative evaluation, including imaging and laboratory studies, helps determine the extent of the disease and guide treatment planning. Complete surgical staging, which involves thorough examination of the pelvic and intra-abdominal structures, is crucial to accurately assess the stage of the tumor and guide further treatment decisions. Optimal tumor debulking, or removing as much of the tumor as possible, improves overall survival and reduces the risk of recurrences.
The specific surgical approach may vary depending on the patient’s fertility desires. In younger patients who desire future fertility, unilateral salpingo-oophorectomy (removal of one ovary and fallopian tube) is usually sufficient treatment. Staging procedures, including pelvic washings, lymph node sampling, biopsies, and examination of the contralateral ovary, are typically performed. The need for lymphadenectomy (removal of lymph nodes) is being questioned due to the low risk of lymph node metastasis even in advanced-stage disease. In younger patients, a dilatation and curettage (D&C) may be considered to rule out a neoplastic process of the endometrium.
For patients who do not require future fertility, surgical therapy should consist of bilateral salpingo-oophorectomy (removal of both ovaries and fallopian tubes) and total abdominal hysterectomy (removal of the uterus), in addition to staging procedures. This comprehensive surgical approach aims to remove all disease and reduce the risk of recurrence.
The treatment of recurrent GCTs is not standardized, and different treatment modalities have been used with varying success. Surgical debulking may be beneficial if the recurrent tumor appears to be focal on imaging studies. Chemotherapy, radiotherapy, and hormonal treatments have also been utilized in the management of recurrent GCTs, but their effectiveness may vary from case to case. The mean survival after a recurrence has been diagnosed is approximately 5 years for adult GCTs, highlighting the importance of closely monitoring patients for recurrence and providing appropriate treatment interventions when necessary.
💡
You may need to know these questions about theca cell tumor
What is a theca cell tumor of the ovaries?
A theca cell tumor of the ovaries is an extremely uncommon type of tumor that makes up less than 1% of all ovarian tumors. It is typically diagnosed in women around the age of 53, although it is rare for women younger than 30 to develop these tumors, except in the case of luteinized thecomas which tend to occur in younger women. These tumors arise from the theca cells, which are responsible for producing hormones such as estrogen and progesterone in the ovaries. When the growth of these cells becomes uncontrolled, it can lead to the development of theca cell tumors. Prompt diagnosis and treatment is crucial for managing these tumors effectively and minimizing potential complications.
How do you treat a theca cell tumor?
The primary approach for addressing theca cell tumors (GCTs) involves surgical intervention. Surgical treatment is considered as the initial line of therapy for patients with these tumors. Chemotherapy and radiotherapy are typically reserved for cases of advanced disease detected through surgical staging or for patients experiencing recurrent tumors. The goal is to remove the tumor through surgical means and utilize chemotherapy or radiotherapy as adjunct therapies when necessary.
What is the difference between a thecoma and a theca cell tumor?
Thecoma and theca cell tumors are both types of ovarian tumors, but they differ in their potential for malignancy. Theca cell tumors are typically benign and have a favorable outlook. On the other hand, theca cell tumors with a small amount of granulosa cells can exhibit malignancy, although they are extremely rare. Overall, the main distinction lies in the prognosis, with thecoma being mostly benign and theca cell tumors with granulosa cells having a higher likelihood of being malignant.
What are the symptoms of theca cell tumor?
Theca cell tumors, such as granulosa theca cell tumors, display a range of symptoms that can vary from person to person. Typically, these tumors affect individuals across a wide age range, spanning from teenagers to the elderly, but are more frequently observed in postmenopausal women aged between 45 to 55 years. The symptoms they present with are usually nonspecific, often consisting of abdominal pain (41.1% of cases), abdominal distension (26.4% of cases), or the presence of a palpable mass in the abdominopelvic region that is typically found on one side. As these symptoms are not exclusive to theca cell tumors, it is essential for medical professionals to conduct appropriate diagnostic tests to confirm the presence of this condition and provide appropriate treatment.
Reference source
https://www.ncbi.nlm.nih.gov/books/NBK565872/
https://emedicine.medscape.com/article/254489-overview
https://emedicine.medscape.com/article/254489-treatment
https://my.clevelandclinic.org/health/diseases/24245-granulosa-cell-tumor