Imagine a world where your body betrays you, where the very foundations of your femininity crumble.
Welcome to the realm of uterine prolapse, a bittersweet reality that engulfs nearly half of women aged 50-79.
Weakened muscles and tissue pave the way for this bewildering condition, bringing with it a myriad of symptoms and challenges.
Brace yourself as we delve into this fascinating world, where the battle for control begins in the most intimate of spaces.
uterine prolapse
Uterine prolapse is a condition characterized by the dropping of the uterus into the vagina due to weakened muscles and tissue in the pelvis.
It affects nearly half of all women between the ages of 50 and 79.
The primary cause of uterine prolapse is the inability of the pelvic floor muscles and tissue to support the weight of the uterus.
Risk factors include giving birth, particularly through vaginal delivery, menopause, being Caucasian, being overweight, and smoking.
While many women with uterine prolapse may not experience any symptoms, possible symptoms include urinary leakage, difficulty emptying the bladder completely, a feeling of heaviness or fullness in the pelvis, vaginal bulging, lower back pain, aching or pressure in the lower abdomen or pelvis, and constipation.
Diagnosis is typically done through a physical examination, possibly supplemented with a cystoscopy to examine the bladder and urethra, as well as an MRI to assess the condition of other pelvic organs such as the kidneys.
Key Points:
- Uterine prolapse occurs when the uterus drops into the vagina due to weakened muscles and tissue in the pelvis.
- It is common among women between the ages of 50 and 79.
- The main cause is the inability of the pelvic floor muscles and tissue to support the weight of the uterus.
- Risk factors include giving birth through vaginal delivery, menopause, being Caucasian, being overweight, and smoking.
- Symptoms may include urinary leakage, difficulty emptying the bladder, a feeling of heaviness in the pelvis, vaginal bulging, lower back pain, and constipation.
- Diagnosis is usually made through a physical examination, cystoscopy, and MRI.
uterine prolapse – Watch Video
💡
Pro Tips:
1. Uterine prolapse, also known as pelvic organ prolapse, occurs when the uterus descends or sags into the vaginal canal.
2. Uterine prolapse is more likely to occur in women who have given birth multiple times.
3. Women who have uterus prolapse may experience symptoms such as a feeling of pressure or heaviness in the pelvic area, backache, or even difficulty inserting tampons.
4. In rare cases, severe uterine prolapse can cause the uterus to protrude from the opening of the vagina.
5. Uterine prolapse can be prevented or minimized by practicing pelvic floor exercises, maintaining a healthy weight, and avoiding heavy lifting.
Definition Of Uterine Prolapse
Uterine prolapse is a condition that occurs when the muscles and tissue in the pelvis weaken, causing the uterus to drop into the vagina. The pelvic floor muscles and ligaments normally provide support to the uterus, but when they become weak or damaged, they are unable to hold the uterus in its proper position. This can lead to a variety of symptoms and complications, impacting a woman’s quality of life.
Prevalence Of Uterine Prolapse In Women
Uterine prolapse is a common condition, particularly in women between the ages of 50 and 79. It is estimated that nearly half of all women in this age group experience uterine prolapse to some degree. This highlights the importance of understanding the causes, symptoms, and treatment options for this prevalent condition.
- Uterine prolapse is more common in women aged 50 to 79.
- Nearly half of women in this age group experience uterine prolapse.
- Understanding the causes, symptoms, and treatment options is crucial.
Main Cause Of Uterine Prolapse
The main cause of uterine prolapse is weakened muscles and tissue in the pelvic floor. These muscles and ligaments play a crucial role in supporting the weight of the uterus. However, factors such as:
- Childbirth
- Vaginal delivery
- Menopause
- Being Caucasian
- Being overweight
- Smoking
can contribute to the weakening of these muscles. As a result, the uterus can descend into the vagina, causing prolapse.
Risk Factors For Uterine Prolapse
Several risk factors have been identified for uterine prolapse. The highest risk factor is giving birth, especially through vaginal delivery. The process of childbirth can stretch and weaken the pelvic floor muscles, increasing the likelihood of uterine prolapse. Additionally, menopause, being Caucasian, being overweight, and smoking are also associated with an increased risk of developing uterine prolapse.
Understanding these risk factors is essential for early detection and prevention.
- Giving birth, especially through vaginal delivery
- Menopause
- Being Caucasian
- Being overweight
- Smoking
“Understanding these risk factors is essential for early detection and prevention.”
Symptoms Of Uterine Prolapse
Women with uterine prolapse may experience a range of symptoms, such as:
- Urinary incontinence: Leakage of urine.
- Incomplete bladder emptying: Inability to completely empty the bladder.
- Pelvic heaviness or fullness: Feeling of heaviness or fullness in the pelvis.
- Vaginal bulging: Sensation of a bulge in the vagina.
- Lower back pain: Pain in the lower back.
- Lower abdominal or pelvic aching: Aching or pressure in the lower abdomen or pelvis.
- Constipation: Difficulty in passing stools.
It is essential for women to be aware of these symptoms and to seek medical attention if they arise.
Note: Uterine prolapse is a condition in which the uterus descends into or protrudes out of the vagina due to weakened pelvic floor muscles and ligaments.
Lack Of Symptoms In Some Women
Interestingly, not all women with uterine prolapse experience noticeable symptoms. Some women may have a mild prolapse that does not cause any discomfort or visible changes. However, even in the absence of symptoms, it is crucial for women to be aware of the condition and undergo regular medical examinations to catch any potential issues early on.
Diagnosis Of Uterine Prolapse
Diagnosing uterine prolapse typically involves a thorough physical exam by a healthcare professional. During the exam, the doctor may assess the positioning of the uterus and evaluate the strength of the pelvic floor muscles. In some cases, additional diagnostic tools such as a cystoscopy or an MRI may be recommended to gain a better understanding of the condition and its impact on the surrounding organs.
- Physical exam by a healthcare professional.
- Assessment of the positioning of the uterus.
- Evaluation of the strength of pelvic floor muscles.
- Additional diagnostic tools may include cystoscopy or MRI.
“Diagnosing uterine prolapse typically involves a thorough physical exam by a healthcare professional. During the exam, the doctor may assess the positioning of the uterus and evaluate the strength of the pelvic floor muscles. In some cases, additional diagnostic tools such as a cystoscopy or an MRI may be recommended to gain a better understanding of the condition and its impact on the surrounding organs.”
Physical Exam For Uterine Prolapse
The physical exam for uterine prolapse involves a thorough examination of the pelvic region. The doctor may visually assess the position and appearance of the uterus and examine the strength of the pelvic floor muscles. This exam is crucial in providing a preliminary assessment of the condition and helping formulate an appropriate treatment plan.
- The exam involves a thorough examination of the pelvic region.
- Visual assessment of the position and appearance of the uterus.
- Examination of the strength of the pelvic floor muscles.
- It helps in formulating an appropriate treatment plan.
“The physical exam for uterine prolapse is a crucial step in assessing the condition and determining the best course of treatment.”
Cystoscopy For Uterine Prolapse Diagnosis
A cystoscopy may be recommended to evaluate the bladder and urethra more thoroughly. During this procedure, a thin tube called a cystoscope, equipped with a camera, is inserted into the urethra to visualize the interior of the bladder. It is useful for identifying urinary abnormalities or complications related to uterine prolapse.
- A cystoscopy is a procedure to evaluate the bladder and urethra.
- It involves using a thin tube called a cystoscope with a camera.
- The cystoscope is inserted into the urethra to visualize the inside of the bladder.
- It can help identify urinary abnormalities and complications associated with uterine prolapse.
MRI For Uterine Prolapse Diagnosis
An MRI, or magnetic resonance imaging, can be used to gain a more detailed understanding of uterine prolapse. This imaging technique provides comprehensive images of the pelvic region, including the kidneys and other pelvic organs. It can assist in accurate diagnosis, treatment planning, and monitoring the progression of the condition.
Uterine prolapse is a prevalent condition that affects a significant number of women.
To effectively manage and treat uterine prolapse, it is important to understand the causes, symptoms, and diagnostic methods associated with the condition. By recognizing the risk factors and implementing preventive strategies, women can take control of their pelvic health. Regular medical check-ups and seeking timely intervention can help manage and alleviate the symptoms associated with uterine prolapse, improving the overall quality of life for women affected by this condition.
Bullet points:
- MRI imaging provides detailed information on uterine prolapse and the pelvic region.
- Uterine prolapse is a prevalent condition affecting women.
- Understanding the causes, symptoms, and diagnostic methods is crucial for effective treatment.
- Recognizing risk factors and implementing preventive strategies is important.
- Regular medical check-ups and timely intervention can help manage and alleviate symptoms.
💡
You may need to know these questions about uterine prolapse
What are the signs of a prolapsed uterus?
Signs of a prolapsed uterus may include noticing a protrusion or bulge of tissue from the vaginal opening. This can be accompanied by a sensation of heaviness or pulling in the pelvic area. Additionally, individuals may experience difficulties emptying their bladder completely and may also experience urinary incontinence. These symptoms can indicate a potential prolapsed uterus and should be brought to the attention of a healthcare professional for further evaluation and treatment.
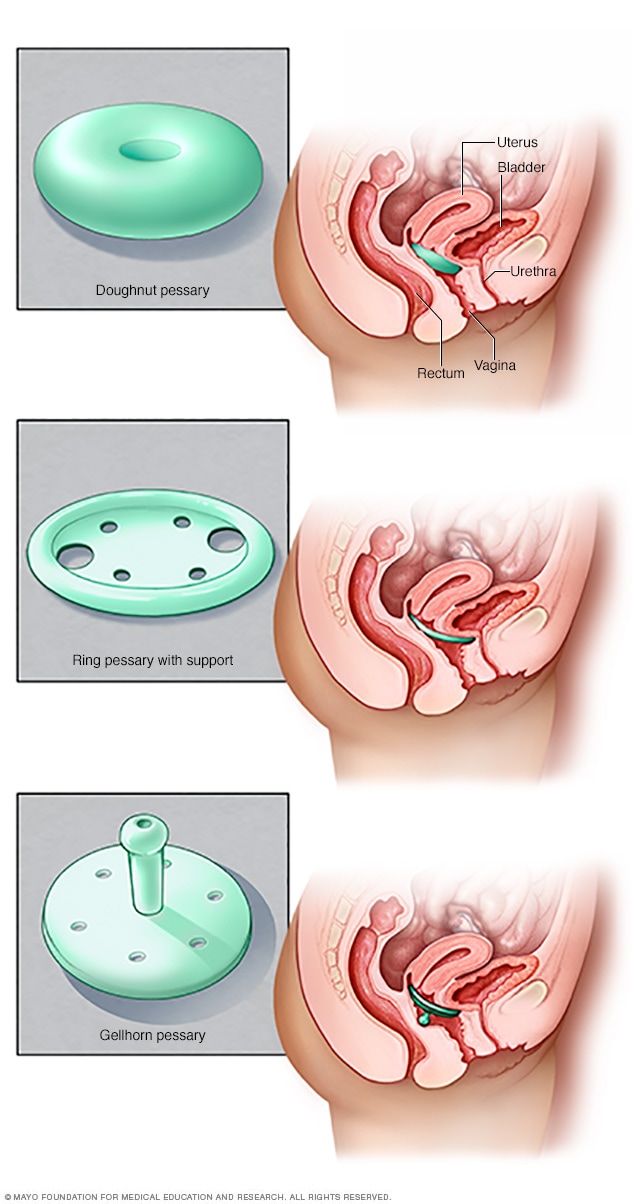
How do you fix a prolapsed uterus?
Repairing the prolapsed uterus typically requires surgical intervention. One possible approach is laparoscopic surgery, a minimally invasive procedure. Another option is vaginal surgery. In cases where uterine prolapse is the only concern, the surgical procedure may involve removing the uterus altogether.
How serious is a prolapsed uterus?
A prolapsed uterus can vary in severity, ranging from mild discomfort to significant hindrances in daily activities. While very mild cases may not cause any discomfort and may not require treatment, severe cases can have a significant impact on a person’s quality of life. In severe instances, it may become difficult to urinate or have a normal bowel movement, which can greatly affect one’s overall well-being. However, with prompt medical attention and appropriate treatment, the seriousness of a prolapsed uterus can be effectively managed.
Is it OK to live with a prolapsed uterus?
In many cases, it is generally considered acceptable to live with a prolapsed uterus. Although it is a prevalent condition affecting a significant portion of women, treatment may not always be necessary. Research from the Women’s Health Initiative suggests that about 40 percent of women in the age group of 50 to 79 have some form of prolapse, highlighting its common occurrence. While some women may experience discomfort or symptoms that significantly impact their quality of life, others may not require immediate medical intervention. Ultimately, the decision to seek treatment should be based on individual circumstances and the advice of a healthcare professional.
Reference source
https://www.hopkinsmedicine.org/health/conditions-and-diseases/uterine-prolapse
https://www.mayoclinic.org/diseases-conditions/uterine-prolapse/symptoms-causes/syc-20353458
https://www.mayoclinic.org/diseases-conditions/uterine-prolapse/diagnosis-treatment/drc-20353464
https://my.clevelandclinic.org/health/diseases/16030-uterine-prolapse