In a world where medical advancements have transformed countless lives, there remains a silent struggle faced by many women.
Vesico-vaginal fistula, a condition often overlooked, can dramatically impact the physical and emotional well-being of those affected.
Join us on a journey to uncover the untold stories and shed light on this deeply important issue.
vesico-vaginal fistula
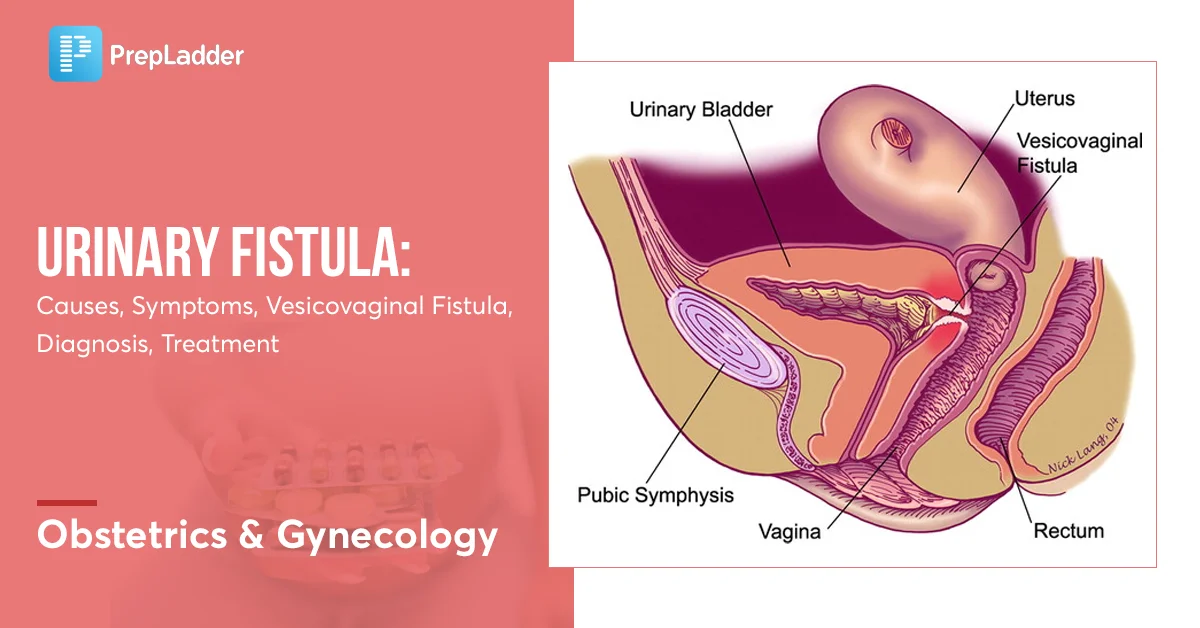
A vesico-vaginal fistula is a medical condition characterized by an abnormal connection or passageway between the bladder and the vagina.
This condition can result in the leakage of urine from the bladder into the vagina, causing significant discomfort and distress for those affected.
It commonly occurs due to obstetric or surgical trauma, but can also be caused by radiation therapy, infection or inflammatory conditions.
Treatment for vesico-vaginal fistula usually involves surgical repair to close the abnormal connection and restore normal urinary function.
Key Points:
- Vesico-vaginal fistula is an abnormal connection or passageway between the bladder and the vagina.
- This condition leads to urine leakage from the bladder into the vagina, causing discomfort and distress.
- Vesico-vaginal fistula is often caused by obstetric or surgical trauma, radiation therapy, infection, or inflammatory conditions.
- Treatment for this condition typically involves surgical repair.
- The goal of treatment is to close the abnormal connection and restore normal urinary function.
- Vesico-vaginal fistula causes significant discomfort and distress for those affected.
vesico-vaginal fistula – Watch Video
💡
Pro Tips:
1. Vesico-vaginal fistula (VVF) is a medical condition characterized by an abnormal connection between the bladder and the vagina.
2. VVF can occur as a result of prolonged labor during childbirth, when the pressure of the baby’s head on the mother’s pelvis can damage the tissues separating the bladder and vagina.
3. The first successful surgical repair of a VVF was performed in the year 1852 by Dr. James Marion Sims, an American physician often referred to as the “father of modern gynecology.”
4. Fistulas were historically stigmatized and considered shameful, leading many women with VVF to become ostracized by their communities due to uncontrollable urine leakage.
5. Organizations such as the Fistula Foundation work tirelessly to raise awareness about VVF and provide surgical interventions to affected women in low-resource countries, where access to proper healthcare may be limited.
1. Introduction To Vesico-Vaginal Fistula
Vesico-vaginal fistula (VVF) is a distressing medical condition that affects women. It is an abnormal connection that forms between the bladder and the vagina, leading to the continuous flow of urine from the bladder into the vagina.
This condition is usually caused by obstetric trauma during childbirth, particularly when prolonged or obstructed labor occurs without access to timely and appropriate medical care.
VVF can have significant physical, psychological, and social impacts on affected women.
- VVF is a distressing medical condition affecting women
- It is an abnormal connection between the bladder and the vagina
- Causes continuous flow of urine from the bladder into the vagina
- Mainly caused by obstetric trauma during childbirth
- Prolonged or obstructed labor without proper medical care
- Significantly impacts women physically, psychologically, and socially.
“Vesico-vaginal fistula is a distressing medical condition that affects women.”
2. Causes Of Vesico-Vaginal Fistula
The primary cause of vesico-vaginal fistula is prolonged or obstructed labor during childbirth. When the baby’s head is not able to pass through the birth canal, pressure builds up, leading to tissue damage and the formation of an abnormal connection between the bladder and vagina.
Other causes of VVF include:
- Pelvic surgery
- Radiation therapy
- Pelvic trauma
- Infection
- Certain gynecological procedures
Factors such as poverty, lack of access to healthcare, and low educational status also increase the risk of developing VVF.
- Prolonged or obstructed labor
- Tissue damage and abnormal connection between the bladder and vagina
- Pelvic surgery
- Radiation therapy
- Pelvic trauma
- Infection
- Certain gynecological procedures
- Factors such as poverty, lack of access to healthcare, and low educational status
3. Symptoms And Signs Of Vesico-Vaginal Fistula
The symptoms and signs of vesico-vaginal fistula can vary in severity depending on the size and location of the fistula. The most common symptom is the involuntary leakage of urine through the vagina, which can be constant or intermittent. This can lead to hygiene issues, discomfort, and embarrassment for affected women.
Other symptoms that may arise include:
- Recurrent urinary tract infections
- Urinary urgency
- Frequent urination
- Dribbling of urine
In severe cases, women may also experience:
- Vaginal discharge
- Foul odor
- Irritation
It is important to note that these symptoms require medical attention. Vesico-vaginal fistula can significantly impact a woman’s quality of life, and timely treatment is essential to address the physical and emotional effects.
“Vesico-vaginal fistula can have profound consequences for affected women, leading to challenges with personal hygiene and social interactions. Prompt medical intervention is vital to restore their health and dignity.”
4. Diagnosis Of Vesico-Vaginal Fistula
Diagnosing vesico-vaginal fistula involves several steps:
-
Thorough medical history: The healthcare provider will inquire about symptoms, childbirth history, and any previous pelvic surgeries or trauma.
-
Physical examination: A pelvic examination will be conducted to assess the area of the fistula.
-
Specialized tests: Additional tests, including urine analysis, cystoscopy, and imaging studies (such as ultrasound or MRI), may be ordered to:
-
Confirm the diagnosis
- Determine the size and location of the fistula
- Assess the surrounding structures
It is crucial to go through these diagnostic procedures to accurately identify and evaluate vesico-vaginal fistula.
5. Treatment Options For Vesico-Vaginal Fistula
The treatment of vesico-vaginal fistula depends on several factors, including:
- Size, location, and severity of the fistula
- Overall health of the patient
Conservative management options may include:
- Use of vaginal tampons, pessaries, or urethral inserts to temporarily control urine leakage
However, surgical repair is the definitive treatment for VVF. In some cases, multiple surgeries or more complex procedures may be required to achieve a successful repair.
Post-surgical care, including regular follow-up visits and monitoring, is essential for optimal outcomes.
‒ Conservative management options:
- Vaginal tampons
- Pessaries
- Urethral inserts
‒ Surgical repair is the definitive treatment for VVF.
- Multiple surgeries or more complex procedures may be required.
‒ Post-surgical care is essential for optimal outcomes:
- Regular follow-up visits and monitoring
6. Surgical Procedures For Repairing Vesico-Vaginal Fistula
There are several surgical procedures available for repairing vesico-vaginal fistula (VVF), and the choice depends on the specific characteristics of the defect. The most common surgical technique is the transvaginal approach, where the fistula is repaired through the vaginal opening. This technique allows direct access to the fistula and avoids the need for an abdominal incision.
In some cases, more complex fistulas may require additional approaches, such as the transabdominal approach or the use of minimally invasive techniques. The choice of procedure is determined by the surgeon’s expertise and individual patient factors.
- Transvaginal approach is the most common surgery for VVF repair
- Allows direct access to the fistula
- Avoids the need for an abdominal incision
“The choice of procedure is determined by the surgeon’s expertise and individual patient factors.”
7. Complications And Risks Associated With Vesico-Vaginal Fistula
Vesico-vaginal fistula (VVF) can have several complications and risks if left untreated or inadequately managed. These include urinary tract infections, which can be recurrent and may lead to kidney damage if not treated promptly. Additionally, VVF can cause physical discomfort, pain during sexual intercourse, and vaginal infections. The constant leakage of urine can also lead to skin irritation and ulcerations on the vaginal and perineal areas, increasing the risk of infections. Psychologically, VVF can significantly impact a woman’s self-esteem, body image, and overall quality of life.
8. Prevention Strategies For Vesico-Vaginal Fistula
Preventing vesico-vaginal fistula requires a multifaceted approach that addresses several key factors. To effectively tackle this issue, the following actions can be taken:
-
Improving access to skilled healthcare professionals: In order to prevent and manage VVF, it is crucial to ensure that skilled healthcare professionals are readily available, particularly in low-resource settings. This will allow for timely interventions during childbirth and reduce the risk of developing fistulas.
-
Enhancing access to emergency obstetric care: In addition to skilled healthcare professionals, it is essential to improve access to emergency obstetric care. This includes facilities equipped to handle emergency deliveries and provide necessary interventions to prevent or repair fistulas.
-
Raising awareness through education programs: Educating women and communities about the importance of timely medical care is a vital step in preventing VVF. This can be accomplished through targeted education and awareness programs that highlight the potential risks associated with prolonged labor. Informing women about the benefits of seeking medical assistance during childbirth can help prevent fistulas from occurring.
-
Empowering women with knowledge on family planning and prenatal care: Empowering women with knowledge about family planning and prenatal care is another crucial aspect of VVF prevention. By offering women information on various contraceptives and family planning methods, they can make informed choices that allow for better management of their reproductive health. Additionally, educating women about the benefits of receiving prenatal care can help identify and address any complications early on, reducing the risk of developing fistulas.
-
Promoting healthcare facility deliveries: Encouraging women to deliver in healthcare facilities can significantly contribute to the prevention of VVF. Providing information about the advantages of delivering in a healthcare facility, such as access to skilled healthcare professionals and emergency obstetric care, can help reduce the occurrence of fistulas.
By implementing these measures, we can work towards the prevention of vesico-vaginal fistula and improve the overall reproductive health of women in affected areas.
- Improving access to skilled healthcare professionals
- Enhancing access to emergency obstetric care
- Raising awareness through education programs
- Empowering women with knowledge on family planning and prenatal care
- Promoting healthcare facility deliveries
9. Psychological And Social Impacts Of Vesico-Vaginal Fistula
The psychological and social impacts of vesico-vaginal fistula (VVF) can have a profound and devastating effect on affected women. The constant leakage of urine and associated odor are not only physically uncomfortable but can also result in social isolation, stigmatization, and rejection by their communities.
Women living with VVF often experience low self-esteem, depression, anxiety, and decreased sexual satisfaction. They may feel overwhelmed by the physical discomfort and fear judgment from others.
The psychological and social consequences of VVF emphasize the critical need for holistic care that not only addresses the physical aspects but also prioritizes the emotional and mental well-being of these women.
- The constant leakage of urine and associated odor can lead to social isolation and stigmatization
- Women with VVF may experience low self-esteem, depression, anxiety, and decreased sexual satisfaction
- Holistic care should focus on addressing the emotional and mental well-being of women living with VVF.
“The psychological and social consequences of vesico-vaginal fistula highlight the importance of providing holistic care that addresses the emotional and mental well-being of women living with VVF.”
10. Support And Resources For Individuals With Vesico-Vaginal Fistula
Multiple organizations and support groups are dedicated to helping women with vesico-vaginal fistula. These organizations provide medical, surgical, and psychosocial support to affected women through specialized healthcare facilities. They offer services such as free surgical interventions, post-operative care, counseling, skills training, and community reintegration programs. Additionally, they advocate for policy changes, increased awareness, and improved access to quality healthcare for underprivileged women in countries affected by VVF. Together, these initiatives aim to restore dignity, improve quality of life, and empower women affected by vesico-vaginal fistula.
💡
You may need to know these questions about vesico-vaginal fistula
What is Vesico cervical fistula?
Vesico-cervical fistula (VCF) is a highly uncommon complication that can occur following a cesarean section (CS). While vesico-uterine fistula (VUF) accounts for approximately 1-4% of genitourinary fistula cases, VCF remains a sporadic occurrence with only a few reported cases. VCF refers to an abnormal connection between the bladder and the cervix, leading to the passage of urine into the cervical canal. It is essential to diagnose and treat VCF promptly to prevent further complications and ensure the well-being of the patient.
What is the most common cause of Vesicouterine fistula?
The most common cause of vesicouterine fistula is typically attributed to cesarean section in the United States. However, other factors such as intrauterine contraceptive devices, tumors, traumatic labor, radiation therapy, or iatrogenic causes like traumatic catheterizations, can also lead to the development of vesicouterine fistulas, albeit less frequently observed.
How do you fix a vesico-uterine fistula?
One way to repair a vesico-uterine fistula is through a surgical approach called transperitoneal access. This method is often considered the most effective with the lowest relapse rate. The surgeon gains access through the abdomen, allowing for a clear view and better manipulation of the affected tissues, ensuring a thorough repair of the fistula. With this approach, the surgeon can safely and efficiently fix the vesico-uterine fistula, helping restore normal urinary and reproductive function for the patient.
How do you treat a Vesicorectal fistula?
The treatment for a Vesicorectal fistula typically involves a surgical approach, with the specific technique determined by the location of the fistula and the patient’s overall health. The choice between a single- or two-stage repair is made based on these factors. While surgical intervention is usually necessary, in some cases, non-operative management may be considered for certain patients who have intravenous total parenteral nutrition, bowel rest, and receive antibiotics. However, this option is only appropriate for a select group of individuals.
Reference source
https://medcraveonline.com/MOJWH/vesico-cervical-fistulae-case-series.html
https://appliedradiology.com/articles/vesicouterine-fistula
https://pubmed.ncbi.nlm.nih.gov/12899224/
https://my.clevelandclinic.org/health/diseases/16442-vesicovaginal-fistula