Discover the mysterious world of vesicular moles, an enigmatic condition that baffles experts and captivates curious minds.
Journey with us as we unravel the secrets behind this intriguing phenomenon, delving into its symptoms, causes, and treatment options.
Brace yourself for a captivating exploration of this unique condition and its complicated web of complications.
vesicular mole
A vesicular mole, also known as a hydatidiform mole, is a rare condition that occurs during pregnancy.
It is characterized by an abnormal growth of placental tissue, leading to the formation of grape-like clusters of fluid-filled sacs, called vesicles.
This condition can result from problems with the fertilization process or abnormalities in the genetic material of the fetus.
Vesicular moles can cause symptoms such as vaginal bleeding, enlarged uterus, and high levels of a hormone called human chorionic gonadotropin (hCG).
Early diagnosis and treatment are important to prevent complications such as choriocarcinoma, a type of cancer that can develop from a vesicular mole.
Treatment usually involves a procedure called dilation and curettage (D&C) to remove the abnormal tissue.
It’s crucial for individuals experiencing symptoms or at risk for vesicular moles to seek medical attention for proper evaluation and management.
Key Points:
- Vesicular mole is a rare condition that occurs during pregnancy characterized by abnormal growth of placental tissue and formation of fluid-filled sacs.
- The condition can result from fertilization problems or abnormalities in the genetic material of the fetus.
- Symptoms of vesicular moles include vaginal bleeding, enlarged uterus, and high levels of hCG.
- Early diagnosis and treatment are important to prevent complications such as choriocarcinoma, a type of cancer.
- Treatment usually involves a procedure called dilation and curettage (D&C) to remove the abnormal tissue.
- Medical attention should be sought by individuals experiencing symptoms or at risk for vesicular moles.
vesicular mole – Watch Video
💡
Pro Tips:
1. Vesicular moles are a type of pregnancy-related tumor that primarily develop in the placenta rather than the mother’s body.
2. In rare instances, vesicular moles can contain developing embryo-like structures, giving them a peculiar resemblance to a bunch of grapes.
3. Vesicular moles are often associated with a hormonal imbalance called gestational trophoblastic disease (GTD), which can lead to abnormal growth of placental cells.
4. Due to their uterine location and resemblance to a normal pregnancy, vesicular moles can be misdiagnosed as an ectopic pregnancy (a pregnancy that occurs outside the uterus).
5. While vesicular moles are typically benign, in some cases they can progress to a more aggressive form of GTD called choriocarcinoma, which requires immediate treatment.
Symptoms Of Vesicular Mole
Vesicular moles, also known as hydatidiform moles, are uncommon gestational trophoblastic diseases that occur during pregnancy. They develop when there is an abnormal fertilization of the egg during conception, resulting in the growth of abnormal placental tissue. Understanding the symptoms of vesicular mole is essential for early diagnosis and timely intervention.
The most common symptom of a vesicular mole is vaginal bleeding, which may be lighter or heavier than a regular menstrual period. Other symptoms may include severe nausea and vomiting that is not alleviated by the typical remedies, such as antacids or rest. Women with vesicular moles may also experience abnormally high blood pressure (preeclampsia), anemia, and an enlarged uterus. Additionally, a grape-like cluster of fluid-filled sacs may be present in the uterus during an ultrasound examination.
Prompt medical attention is crucial for an accurate diagnosis and appropriate management.
- Vaginal bleeding (lighter or heavier than normal)
- Severe nausea and vomiting
- Abnormally high blood pressure (preeclampsia)
- Anemia
- Enlarged uterus
- Grape-like cluster of fluid-filled sacs in the uterus during ultrasound examination
Treatment Options For Vesicular Mole
Once a vesicular mole is diagnosed, prompt and appropriate treatment is necessary to minimize complications and maintain the health of the mother. The primary treatment for vesicular moles is the removal of the abnormal tissue through a procedure called suction dilation and curettage (D&C). During this procedure, the cervix is dilated, and the molar tissue is gently suctioned out. In some cases, a hysteroscopy may be performed to visualize the uterus and ensure complete removal of the mole.
Following the removal of the vesicular mole, close monitoring of hCG (human chorionic gonadotropin) levels is crucial. Regular blood tests are conducted to check the hCG levels, as elevated or persistently high levels may indicate remaining molar tissue or the development of a more aggressive form of gestational trophoblastic disease, such as choriocarcinoma.
In cases where the vesicular mole is extensive or if choriocarcinoma is suspected, additional treatment options may be required. This may include chemotherapy or radiation therapy to eliminate any remaining abnormal cells and reduce the risk of recurrence or metastasis.
Diagnosing Vesicular Mole
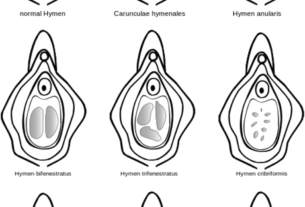
Accurate and timely diagnosis is essential for effective management of vesicular moles. Diagnosis usually begins with a thorough medical history and physical examination, including a pelvic exam. However, definitive diagnosis is typically confirmed through ultrasound imaging.
An ultrasound examination reveals the presence of characteristic features of a vesicular mole, including the absence of a viable fetus or fetal heartbeat. Instead, the ultrasound may reveal a mass of small fluid-filled sacs within the uterus, resembling a cluster of grapes. This appearance is known as a “snowstorm” pattern and is highly suggestive of a vesicular mole.
In some cases, additional diagnostic tests may be performed to confirm the diagnosis and rule out other conditions. This may include blood tests to measure hCG levels, genetic testing of the molar tissue, or imaging studies to assess the extent of the molar growth and potential spread to other organs.
– Ultrasound examination
– Snowstorm appearance
– Blood tests for hCG levels
– Genetic testing of molar tissue
– Imaging studies.
Common Causes Of Vesicular Mole
Vesicular moles occur due to abnormal fertilization of an egg during conception. There are two main types of vesicular moles: complete moles and partial moles.
Complete moles occur when an egg is fertilized by a sperm that contains no genetic material or is inactive. This results in the growth of a placenta without a viable fetus. Partial moles, on the other hand, develop when an egg is fertilized by two sperm or when a normal egg is fertilized by a sperm with duplicated genetic material. In both cases, the genetic abnormalities lead to the growth of abnormal placental tissue.
The exact cause of these genetic abnormalities is still unknown, but certain risk factors may increase the likelihood of developing a vesicular mole. These risk factors include advanced maternal age, previous history of vesicular mole, and a diet low in protein, fruits, and vegetables.
- Advanced maternal age
- Previous history of vesicular mole
- Diet low in protein, fruits, and vegetables.
“Vesicular moles occur due to abnormal fertilization of an egg during conception. There are two main types of vesicular moles: complete moles and partial moles. Complete moles occur when an egg is fertilized by a sperm that contains no genetic material or is inactive. This results in the growth of a placenta without a viable fetus. Partial moles, on the other hand, develop when an egg is fertilized by two sperm or when a normal egg is fertilized by a sperm with duplicated genetic material. In both cases, the genetic abnormalities lead to the growth of abnormal placental tissue.”
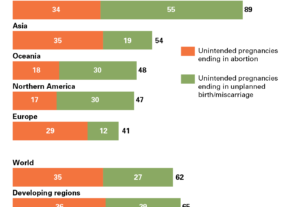
Prevalence Of Vesicular Mole
Vesicular moles, also known as hydatidiform moles, are a relatively rare condition that occurs in approximately 1 in every 1,500 pregnancies in the United States[^1^]. The prevalence of this condition may vary among different populations and geographical regions.
- It is important to note that the incidence of vesicular moles is higher in specific populations, particularly in women from Southeast Asia[^1^].
- Factors such as genetic predisposition and cultural influences may contribute to these differences in prevalence[^1^].
“The incidence of vesicular moles is higher in certain populations, such as women from Southeast Asia.” [^1^]
- The prevalence of vesicular moles is approximately 1 in every 1,500 pregnancies in the United States.
- The incidence may vary in different populations and geographical regions.
Please let me know if you need any further improvements or additions.
Risk Factors For Developing Vesicular Mole
While the exact cause of vesicular moles remains unknown, certain risk factors have been identified. Advanced maternal age, particularly women over the age of 35, is considered a significant risk factor for the development of vesicular moles. Previous history of vesicular mole increases the risk of recurrence in future pregnancies. Additionally, inadequate nutrition, such as a diet low in protein, fruits, and vegetables, has been associated with an increased risk of developing vesicular moles.
It is important for individuals with these risk factors to undergo appropriate prenatal care and screening, as early detection and timely intervention can significantly reduce the potential complications associated with vesicular moles.
- Advanced maternal age (over 35)
- Previous history of vesicular mole
- Inadequate nutrition (low protein, fruits, and vegetables)
“It is important for individuals with these risk factors to undergo appropriate prenatal care and screening, as early detection and timely intervention can significantly reduce the potential complications associated with vesicular moles.”
Potential Complications Of Vesicular Mole
While most vesicular moles can be successfully treated and do not cause long-term problems, there are potential complications that can arise if they are left untreated or if the mole progresses to a more aggressive form of gestational trophoblastic disease.
Complications include:
- Uterine rupture
- Hemorrhage
- Spread of abnormal cells to other organs (lungs, liver, brain)
- Life-threatening situations
In such cases, more aggressive treatment options like chemotherapy or radiation therapy may be required.
Monitoring hCG levels and regular follow-up care are essential to detect and manage any potential complications promptly. Early intervention can significantly improve the prognosis and minimize the risk of long-term complications.
Understanding The Histopathology Of Vesicular Mole
Histopathology refers to the microscopic examination of tissues to study the structural changes and abnormalities. In the case of vesicular moles, histopathology plays a crucial role in confirming the diagnosis and assessing the extent of the molar growth.
A histopathological examination of the molar tissue reveals the absence of viable fetal tissue and the presence of abnormal placental tissue. The placental tissue in vesicular moles typically shows edematous (swollen) villi with the presence of focal or diffuse trophoblastic hyperplasia. The presence of trophoblastic hyperplasia is a key characteristic that distinguishes vesicular moles from other placental abnormalities.
The histopathological findings are essential in guiding the treatment options and providing valuable information regarding the stage and extent of the disease.
Gestational Trophoblastic Disease And Vesicular Mole
Vesicular moles are a type of gestational trophoblastic disease (GTD), which refers to a group of conditions involving abnormal placental tissue growth. GTD includes both benign and malignant conditions, such as vesicular moles, choriocarcinoma, and placental site trophoblastic tumors.
Gestational trophoblastic diseases, including vesicular moles, result from abnormal fertilization events during conception. The placental tissue grows rapidly and can invade the uterine wall or spread to other organs. The diagnosis and management of GTD require thorough evaluation and often involve a multidisciplinary team of obstetricians, gynecologic oncologists, and pathologists.
It is important to note that vesicular moles, though generally benign, can progress to more aggressive forms of gestational trophoblastic disease if left untreated. Regular follow-up care and monitoring of hCG levels are necessary to detect any signs of progression or recurrence.
- Vesicular moles are a type of gestational trophoblastic disease (GTD)
- GTD includes both benign and malignant conditions
- Vesicular moles result from abnormal fertilization events
- The diagnosis and management of GTD require a multidisciplinary team
“It is important to note that vesicular moles, though generally benign, can progress to more aggressive forms of gestational trophoblastic disease if left untreated.”
Differentiating Between Complete And Partial Mole
Vesicular moles can be categorized into two main types: complete moles and partial moles. Differentiating between these two types is crucial for appropriate management and counseling.
Complete moles occur when the egg is fertilized by a sperm that contains no genetic material or is inactive. As a result, the placental tissue develops without a viable fetus. On the other hand, partial moles develop when the egg is fertilized by two sperm or when a normal egg is fertilized by a sperm with duplicated genetic material. In both cases, there is the presence of fetal tissue, although it is typically abnormal.
Distinguishing between complete and partial moles is primarily based on the histopathological examination of the molar tissue. Complete moles typically show a diploid or androgenetic karyotype, indicating that all the genetic material comes from the father. Partial moles, on the other hand, exhibit triploid or hypertriploid karyotypes, indicating an abnormal balance of genetic material from both the mother and the father.
The differentiation between complete and partial moles is important for counseling patients regarding the risk of complications, including choriocarcinoma and future pregnancies. It also assists in determining the appropriate management options, such as the need for additional treatment or closer surveillance.
In conclusion, understanding the complications of vesicular moles is essential for early diagnosis, effective management, and appropriate counseling. Prompt medical attention for symptoms, accurate diagnosis through various diagnostic tests, and timely treatment options are crucial in preventing potential complications and ensuring optimal maternal health. Regular follow-up care and monitoring of hCG levels are necessary to detect any signs of recurrence or progression to more aggressive forms of gestational trophoblastic disease. With early detection and proper management, the prognosis for vesicular moles is generally favorable.
💡
You may need to know these questions about vesicular mole
What is a hydatidiform mole or vesicular mole?
A hydatidiform mole, or vesicular mole, is a rare condition that occurs during pregnancy where the placenta develops into an abnormal growth instead of a fetus. This gestational trophoblastic disease originates from the placenta itself, rather than from maternal tissue. The mole can sometimes metastasize, spreading to other areas of the body. Though it is a non-cancerous tumor, it can exhibit invasive behavior and may require treatment to prevent complications and ensure the health of the patient.
What is the cause of hydatidiform mole?
Hydatidiform mole is caused by an abnormal fertilization process where a normal sperm cell fertilizes an oocyte, leading to an embryo with only one set of chromosomes. Since the embryo lacks genes from the mother, it cannot develop properly, giving rise to a hydatidiform mole. This abnormality disrupts the usual progress of pregnancy and presents a unique challenge for successful embryonic development.
What is the treatment of choice for a vesicular mole?
The treatment of choice for a vesicular mole is typically suction aspiration. This method is commonly preferred due to its efficacy in removing the molar tissue from the uterus. However, in exceptional cases where there are uterine abnormalities present, surgical treatment may not be feasible and alternative approaches could be explored, such as medical management or close monitoring of the condition. These options would need to be determined based on the specific circumstances of each individual case to ensure the best possible outcome for the patient.
Is a hydatidiform mole a miscarriage?
A hydatidiform mole, also known as a molar pregnancy, is not considered a miscarriage. It is a type of abnormal pregnancy where the growth in the uterus is due to the presence of placental cells that develop into a mass, resembling a cluster of grapes. Unlike a miscarriage, which typically occurs due to natural fetal demise, a hydatidiform mole involves the abnormal development of placental tissue. In some cases, a fetus may develop but it will be abnormal and cannot survive for long, up to approximately three months in most instances.
Reference source
https://en.wikipedia.org/wiki/Molar_pregnancy
https://www.ncbi.nlm.nih.gov/books/NBK459155/
https://medlineplus.gov/genetics/condition/recurrent-hydatidiform-mole/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2729468/